fig2
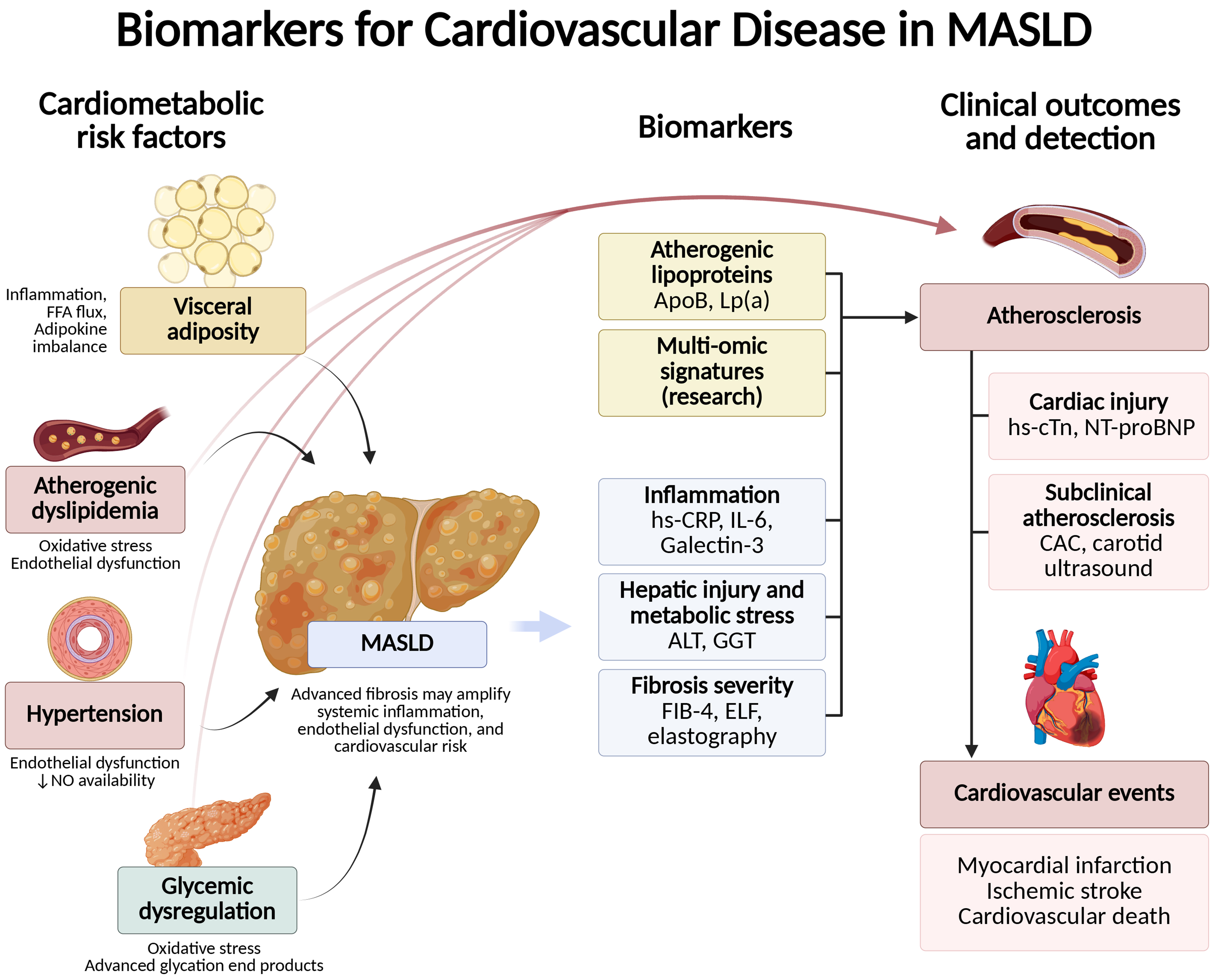
Figure 2. Pathophysiologic framework linking MASLD to CVD, and potential biomarkers. Metabolic dysfunction in MASLD, together with hepatic inflammation and advanced fibrosis, promotes systemic inflammation and vascular injury. These upstream drivers converge on core atherogenic mechanisms - endothelial dysfunction, oxidative stress and lipoprotein modification, macrophage activation with foam-cell formation, plaque growth with calcification, and a prothrombotic milieu - which can be captured by complementary biomarker classes. Created in BioRender. Arab, J. (2025) https://BioRender.com/bka7tlp. MASLD: Metabolic dysfunction-associated steatotic liver disease; CVD: cardiovascular disease; FFA: free fatty acid; NO: nitric oxide; Lp(a): lipoprotein(a); hs-CRP: high-sensitivity C-reactive protein; IL-6: interleukin-6; ALT: alanine aminotransferase; GGT: gamma-glutamyl transferase; FIB-4: Fibrosis-4; ELF: enhanced liver fibrosis; hs-cTn: high-sensitivity cardiac troponin; NT-proBNP: N-terminal pro–B-type natriuretic peptide; CAC: coronary artery calcium.