Combining multiple approaches and omics technologies to detect circulating tumor cells (CTCs): a real clinical application in patients with early-stage non-small-cell lung cancer (NSCLC)?
Abstract
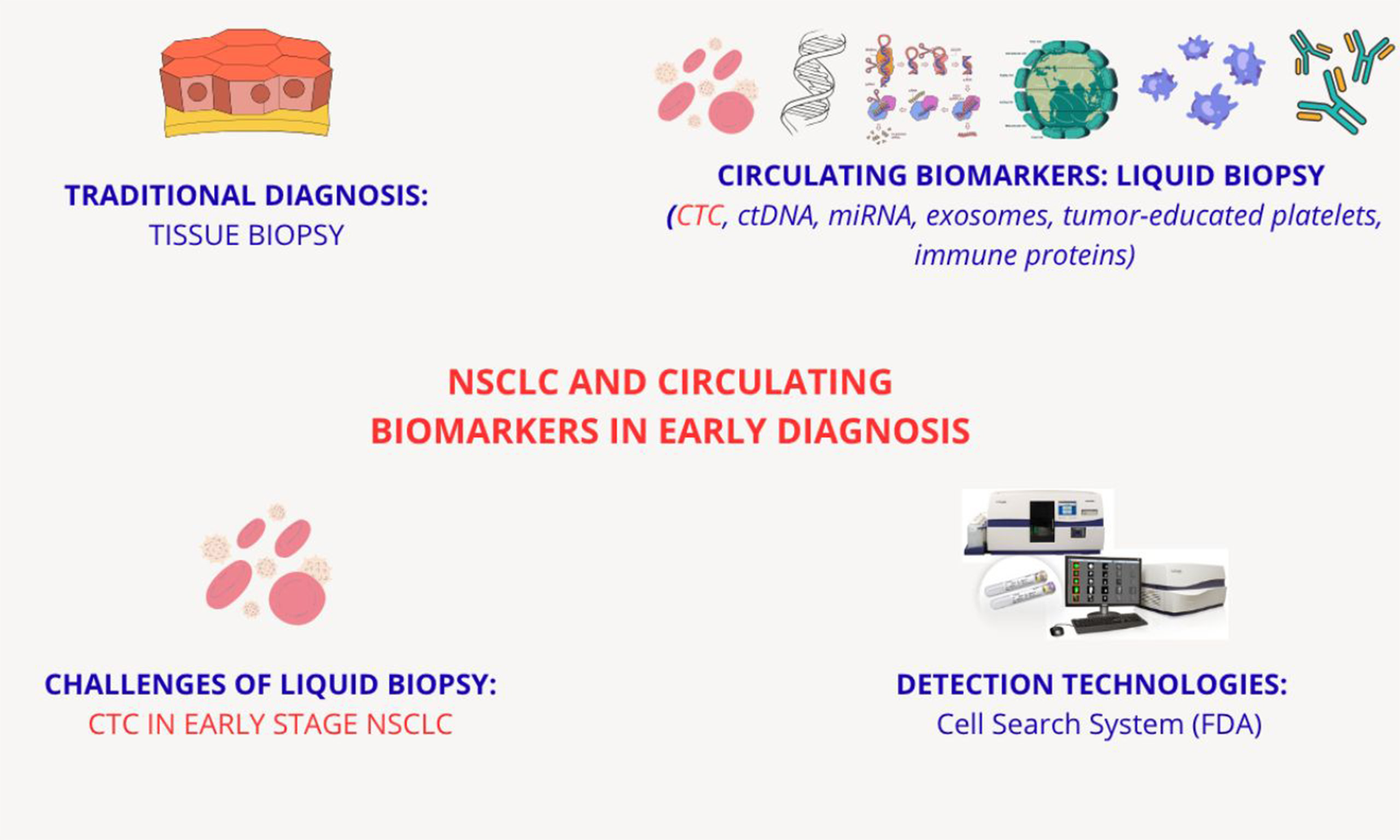
Non-small cell lung cancer (NSCLC) remains one of the most aggressive human malignancies worldwide. While tissue biopsy has long been considered the gold standard for diagnosing NSCLC, the past two decades have seen the emergence of various circulating biomarkers as key components of plasma-based liquid biopsy in NSCLC. These include circulating tumor cells (CTCs), circulating cell-free nucleic acids such as circulating tumor DNA and microRNAs, extracellular vesicles (exosomes), tumor-educated platelets, circulating proteins, and immune cells or immune system components. Despite their promise, CTCs are not yet routinely used in clinical practice for early-stage NSCLC. This commentary highlights the current understanding and detection of CTCs in early-stage NSCLC patients. To date, identifying reliable blood-based biomarkers - whether associated with CTCs or not - remains a major hurdle to diagnosing NSCLC across both early and advanced stages. Monitoring CTC levels could provide important clues on tumor heterogeneity and complexity, including pathologic staging, primary tumor characteristics, and treatment response, particularly in advanced disease. Currently, multiple techniques exist for isolating, characterizing, and enumerating CTCs. Among them, the CellSearch System is the most widely used and remains the only US FDA-approved method, despite certain limitations. In addition, this commentary explores the potential of combining other diagnostic modalities, such as 18-FDG PET/CT, with emerging nanotechnologies to monitor lung nodules - even at early stages - offering deeper insights into disease onset, progression, and therapeutic response.
Keywords
Lung cancer is the main cause of cancer-related death worldwide, with non-small cell lung cancer (NSCLC) accounting for 80%-85% of lung cancer[1]. Unfortunately, most NSCLC patients are diagnosed at an advanced stage[2], with an overall 5-year survival rate of only 20%-25% across all stages[3]. To date, solitary pulmonary nodules can be further evaluated radiologically through second-level imaging techniques to assess key parameters such as lesion size and location[4].
The National Lung Screening Trial, first conducted in the United States in 2011, demonstrated that the implementation of low-dose computed tomography (LDCT) screening significantly increased the detection rate of early-stage lung cancer, thereby reducing the proportion of patients diagnosed at advanced stages[5]. Conventional diagnostic methods for lung cancer include chest X-ray, computed tomography (CT), bronchoscopy, and sputum cytology[6].
Once diagnosed, treatment of NSCLC is often challenging due to high tumor heterogeneity, which promotes therapy resistance and contributes to poor prognosis; therefore, prevention and early detection are key points in effective cancer management. In this context, the 2010 TNM classification introduced a new stage, cM 0 (i+), where the "i +" designation indicates the absence of clinical or radiological evidence of distant metastases but the presence of circulating tumor cells (CTCs) detected microscopically in blood, bone marrow, or tissues outside the regional lymph nodes. These CTCs are typically smaller than 0.2 mm and are found in patients without overt signs or symptoms of metastasis[7].
CTCs were first described in 1869 by pathologist Thomas Ashworth, who identified them in the bloodstream of a deceased cancer patient. CTCs are rare in peripheral blood (occurring at a frequency of approximately 1 per 106-7 leukocytes), and may exist as single cells or in clusters known as circulating tumor microemboli, which can also contain immune cells and platelets[8,9].
Building on this definition, Jiang et al. reported that blood CTC levels are significantly higher in advanced-stage NSCLC patients compared to those with early-stage disease[10]. Therefore, in advanced or metastatic NSCLC, the detection of CTCs can serve as a valuable tool for dynamic monitoring of post-treatment response to distinguish patients at low or high risk of recurrence[11].
However, Wan et al. found that CTCs can also be detected in early-stage (stage I) NSCLC patients
The multicenter cohort study AIR[13] showed that CTC counting in patients with chronic obstructive pulmonary disease (COPD) can help differentiate malignant from benign nodular lesions identified on LDCT. Supporting this, Sun et al. integrated CTC counting using an automated fluorescence microscope with comparative imaging from 18F-FDG PET/CT[14]. This approach employed multiple probes (CK8/18/19, EpCAM, Vimentin, and CD45) to quantify and subtype CTCs, illustrating how LDCT and t 18F-FDG PET/CT can be complemented by molecular diagnostics.
In early-stage NSCLC, is it worth considering whether the presence of CTCs in peripheral blood might bypass routine imaging and represent distant micrometastasis that typically remain undetectable until advanced stages? CTCs may exist in proliferative or quiescent states, and exhibit either epithelial or mesenchymal characteristics[15]. Some also show cancer stem cell-like features, which are believed to contribute to tumor recurrence and metastasis due to their ability to survive in circulation and initiate new tumor growth[16].
This biological heterogeneity, including the persistence of quiescent CTCs in various tissues even after tumor resection, presents significant challenges for researchers. Identifying biomarkers that can detect all CTC subtypes with high sensitivity and specificity remains difficult. Currently known serum tumor markers used for lung cancer diagnosis - such as carcinoembryonic antigen (CEA), cytokeratin fragment-19 (CYFRA21-1), and neuron-specific enolase (NSE) - often yield inconclusive results due to limited specificity[17].
Tissue biopsy is currently the gold standard for cancer diagnosis[18]. However, liquid biopsy is emerging as a minimally invasive and equally valid alternative that may be considered for future guideline inclusion. IN patients with advanced NSCLC, several liquid biopsy markers derived from peripheral blood have been reported in the literature[19]. The most commonly used markers for dynamic and post-treatment monitoring include circulating tumor DNA (ctDNA), CTCs, microRNAs (miRNAs) and extracellular vesicles (EVs). The scope of liquid biopsy has recently expanded to other physiological fluids, such as cerebrospinal fluid, pleural fluid, urine, sputum, and saliva[20].
While CTC count is an established prognostic tool in certain cancers, including breast, prostate, and colorectal cancer, the prognostic value of CTCs in lung cancer remains uncertain[21]. CTCs are released from primary or metastatic lung tumors and enter the bloodstream. Based on the hypothesis that early hematogenous dissemination of CTCs may reflect the risk of disease progression, advanced disease, or overall prognosis, here we focus on the current clinical utility of CTC detection in patients with early-stage NSCLC - a setting in which no standardized detection method is currently available.
Previous studies have investigated CTC detection in cancer patients, noting their short plasma half-life
Clinical and preclinical studies evaluating the use of CTC detection in lung cancer
| References | NSCLC stages | Biomarkers/method | Key findings |
| Leroy et al., 2017[13] | Early & advanced NSCLC | CellSearch and others | Technical challenges reported; mesenchymal CTCs linked to treatment resistance; prognostic value confirmed |
| Hofman et al., 2011[25] | Early-stage NSCLC (I-II) | CTC (CellSearch, EpCAM-based) | Presence of CTCs before surgery was associated with shorter progression-free and overall survival |
| Ilie et al., 2014[26] | Early & Advanced NSCLC (III-IV) | CellSearch | CTC count correlated with survival and treatment response; limitations noted in detecting EMT-CTCs |
| Zhang et al., 2022[42] | Early & Advanced NSCLC | Microfluidic platform | High sensitivity for both epithelial and mesenchymal CTCs; molecular profiling supports therapeutic decision making |
| Abramson Cancer Center at Penn Medicine[46] | Stage I | Microfluidic platform | CTCS demonstrated potential as a non-invasive method for confirming pathological diagnosis in early-stage NSCLC |
| Jin et al., 2017[47] | Early-stage | CTC | Detection of ≥ 1 preoperative CTC was associated with significantly worse disease-free survival |
| Markou et al., 2023[48] | Early-stage | CTC, cfDNA | CTCs and cfDNA provided molecular insights relevant for prognosis |
The CellSearch® CTC test (Menarini-Silicon Biosystems, Bologna, Italy) is currently the only FDA-validated method for the detection of CTCs in the blood of patients with breast, colorectal, and prostate cancer[28,29]. Although the CellSearch® system is known to effectively detect CTCs[30], its performance is not always reliable in NSCLC due to the frequent downregulation of epithelial markers, such as EpCAM, and the phenotypic heterogeneity of NSCLC CTCs[31]. These limitations make it challenging to develop a universally sensitive and specific assay for NSCLC that meets FDA validation standards, unlike in breast, colorectal, and prostate cancers[32].
Rossi et al. conducted a pilot study using a novel morphological measurement approach to detect viable CTCs from pleural lavage samples in individual NSCLC patients[33]. The samples were processed using the CellSearch system. Single-cell light scattering analysis served as the basis for a machine learning (ML) model to characterize the biophysical properties of individual CTCs. Single-cell techniques[34], including mass spectrometry (MS) analysis, preserve the original biological properties of isolated CTCs. However, the rarity of these cells and their weak signal intensity pose challenges for analysis[35].
Briefly, the CellSearch® system is an antigen-based isolation method. In the initial step, EpCAM+CTCs are enriched using immunomagnetic beads conjugated with anti-EpCAM antibodies. This is followed by fluorescent labeling with anti-cytokeratin (CK) antibodies and anti-CD45-allophycocyanin antibodies to exclude leukocytes[36]. The immunomagnetically labeled cells are retained in a magnetic field and analyzed using the CellTracks Analyzer II® (Menarini © Silicon Biosystems)[37].
CTCs can be isolated from blood or pleural effusion relatively easily[38]. Most CTC isolation technologies rely on the detection of epithelial cell surface markers (EpCAM). However, mesenchymal markers - like vimentin - are also expressed by white blood cells, complicating detection. This may limit the ability to identify heterogeneous CTCs, particularly those with stem-like phenotypes or those in varying cellular states (dormant vs proliferative).
According to He et al., a dual-label approach using anti-EpCAM and anti-oncofetal chondroitin sulfate (ofCS) rVAR2-coated magnetic nanoparticles (NC@silica-SA) could provide a more sensitive method for identifying CTCs in the blood of NSCLC patients, employing the FETCH separation system[39]. Previously, Salanti et al. demonstrated the specificity of ofCS, the target of rVAR2, which is absent in healthy lung tissue but present in tumor tissue[40].
Sun et al. reported the presence of CD45+EpCAM+ cells in tumor tissues and malignant pleural fluid of NSCLC patients[41]. Additionally, the proportion of CD45+EpCAM+ cells in the peripheral blood mononuclear cells (PBMCs) of patients was significantly higher than in healthy volunteers (patients: 0.244 ± 0.353 vs. healthy volunteers: 0.012 ± 0.004). Combining the detection of CD45+EpCAM+ cells in circulation with common serum markers such as CEA and CYFRA21-1 may enhance early-stage NSCLC screening.
Despite the variety of available CTC detection technologies, differences in sensitivity and specificity often hinder the ability to obtain adequate sampling volumes of CTCs[42,43]. Microfluidic devices can rapidly process large blood volumes, making them suitable for detecting rare CTCs. These devices reduce the volume of blood required for analysis, lower reagent costs, and can be designed to be portable and automated. Furthermore, combining different microfluidic techniques, such as size-based separation with immunoaffinity capture, can improve both capture efficiency and the purity of mesenchymal CTCs. Table 2 compares the pros and cons of Cellsearch with those of microfluidics.
CellSearch vs. Microfluidics for CRC detection in lung cancer
| Feature | CellSearch | Microfluidics |
| Target CTC phenotype | Mainly epithelial CTCs (EpCAM positive) | Both epithelial and mesenchymal CTCs (based on physical properties and multiple markers) |
| Sensitivity in early NSCLC | Low; difficult to detect due to low EpCAM expression | Higher sensitivity; capable of detecting mesenchymal and heterogeneous CTC phenotypes |
| Turnaround time | Approximately 1-3 days | Approximately 1-3 days |
| Cost | Moderate (~700-1,500 EUR/test) | Variable; generally higher due to technical complexity |
| Advantages | Standardized, FDA-approved, widely used clinically | High sensitivity, detailed phenotypic/molecular profiling, detects rare/relevant cells |
| Limitations | Cannot detect mesenchymal CTCs; false-negative risk in early stages | Technically complex, high costs, not yet standardized for clinical use |
As an example, Ye et al. designed a microfluidic chip featuring well-arranged micropillars within the channel[44]. This device enables the separation of leukocytes from blood samples using CD45 antibodies, removal of smaller cells via a nanofiltration membrane, and classification of isolated CTCs through a fluorescence staining system. Furthermore, biomarker-independent strategies employing surface-charged superparamagnetic nanoprobes are emerging as effective tools for capturing diverse CTC subpopulations[45-48].
Recently, surgical specimens of primary lung tumors have been used to establish lung cancer organoids (LCOs)[49,50]. Several studies have also reported innovative methodologies for isolating CTCs to generate CTC-derived organoids[51-55], as described by De Renzi et al. in small cell lung cancer (SCLC) patients[56]. Hamilton et al. demonstrated that a high CTC count is significantly associated with poorer prognosis in SCLC[57]. These 3D patient-derived organoids replicate the heterogeneity and structural complexity of tumors - including intratumoral diversity and interactions with the microenvironment - and, importantly, can be expanded in vitro or in vivo in mice. However, only a few such studies have been conducted in NSCLC patients. A summary of key studies on CTC-derived organoids or xenografts in lung cancer is provided in Table 3.
Summary of key published studies or abstracts/posters on the generation of CTC-derived organoids in non-small cell lung cancer (NSCLC), comparing early-stage (I-III) and advanced-stage (III-IV or metastatic) patients
| References | NSCLC stage | No. of patients | Culture method | Success rate | Main findings |
| Zhang et al., 2014[43] | Early (Stage I-III)/Advanced | 19 early-stage/7 advanced-stage patients | Microfluidic CTC isolation + 3D co-culture with fibroblasts | 73% (14/19) in early stage | CTCs expanded ex vivo; organoids used for drug testing and molecular profiling; protocol also applied to advanced-stage patients |
| Lin et al., 2018[53] | Advanced | No human patients | CTC injection into mice tumor formation (CDX model) | 50%-70% reduction in tumor size | In vivo tumor derived from CTCs; model used to study drug resistance |
| Lahmadi, 2024[54] | Advanced (Stage III-IV) | 20 patients | CTCs from 4 mL blood; 3D culture in Matrigel | 75% (15/20) | Organoids reflected primary tumor mutations (EGFR/KRAS); suitable for drug testing |
| O’Byrne et al., 2020[55] | Advanced/Metastatic | 70 patients (38 with CTC > 2) | Microfluidic chip; short-term culture in hypoxic organoid medium | 13%(9/70) | Short-lived cultures; EGFR/ALK mutations detected; not suitable for long-term use |
In conclusion, NSCLC CTCs often evade detection by traditional epithelial markers such as EpCAM, due to their downregulation and phenotypic heterogeneity. This makes it challenging to develop a universally sensitive and specific assay that meets FDA validation standards, unlike those available for breast, colorectal, and prostate cancers.
We believe that relying on a single biomarker and/or a single detection technology may result in false-negative findings and does not align with the principles of personalized medicine. The lack of reliable blood-based biomarkers remains a major barrier to the diagnosis of NSCLC, in both early and advanced stages. Despite their potential, CTCs are not yet routinely used in clinical practice due to limitations such as low sensitivity, high cost, and a lack of standardization. To advance precision medicine in lung cancer, it is essential to invest in pilot studies that evaluate the real-world clinical application of CTCs in early-stage NSCLC patients. Additionally, retrospective studies involving cohorts of patients with both early- and advanced-stage disease could help move the field forward. Gaining a deeper understanding of the tumor microenvironment - before the onset of metastasis - may enable the development of multimodal diagnostic strategies for early-stage NSCLC.
DECLARATIONS
Authors’ contributions
Project administration: Fiorelli A
Data curation and writing-original draft: Giorgiano NM
Supervision: Pentimalli F
Resources: Morgillo F, Grimaldi AM
All authors have read and agreed to the published version of the manuscript.
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2025.
REFERENCES
1. Bareschino MA, Schettino C, Rossi A, et al. Treatment of advanced non small cell lung cancer. J Thorac Dis. 2011;3:122-33.
2. Cufer T, Ovcaricek T, O'Brien ME. Systemic therapy of advanced non-small cell lung cancer: major-developments of the last 5-years. Eur J Cancer. 2013;49:1216-25.
3. Boccellino M, Pinto F, Ieluzzi V, et al. Proteomics analysis of human serum of patients with non-small-cell lung cancer reveals proteins as diagnostic biomarker candidates. J Cell Physiol. 2019;234:23798-806.
4. Videtic GMM, Donington J, Giuliani M, et al. Stereotactic body radiation therapy for early-stage non-small cell lung cancer: executive Summary of an ASTRO evidence-based guideline. Pract Radiat Oncol. 2017;7:295-301.
5. Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395-409.
6. Gasparri R, Sabalic A, Spaggiari L. The early diagnosis of lung cancer: critical gaps in the discovery of biomarkers. J Clin Med. 2023;12:7244.
7. O'Sullivan B, Brierley J, Byrd D, et al. The TNM classification of malignant tumours-towards common understanding and reasonable expectations. Lancet Oncol. 2017;18:849-51.
8. Hofman V, Ilie M, Long E, et al. Detection of circulating tumor cells from lung cancer patients in the era of targeted therapy: promises, drawbacks and pitfalls. Curr Mol Med. 2014;14:440-56.
10. Jiang SS, Deng B, Feng YG, et al. Circulating tumor cells prior to initial treatment is an important prognostic factor of survival in non-small cell lung cancer: a meta-analysis and system review. BMC Pulm Med. 2019;19:262.
11. Qian H, Zhang Y, Xu J, He J, Gao W. Progress and application of circulating tumor cells in non-small cell lung cancer. Mol Ther Oncolytics. 2021;22:72-84.
12. Wan JW, Gao MZ, Hu RJ, et al. A preliminary study on the relationship between circulating tumor cells count and clinical features in patients with non-small cell lung cancer. Ann Transl Med. 2015;3:352.
13. Leroy S, Benzaquen J, Mazzetta A, et al. Circulating tumour cells as a potential screening tool for lung cancer (the AIR study): protocol of a prospective multicentre cohort study in France. BMJ Open. 2017;7:e018884.
14. Sun M, Lu D, Li X, et al. Combination of circulating tumor cells and 18F-FDG PET/CT for precision diagnosis in patients with non-small cell lung cancer. Cancer Med. 2024;13:e70216.
15. Valastyan S, Weinberg RA. Tumor metastasis: molecular insights and evolving paradigms. Cell. 2011;147:275-92.
16. Yang MH, Imrali A, Heeschen C. Circulating cancer stem cells: the importance to select. Chin J Cancer Res. 2015;27:437-49.
17. Jiang ZF, Wang M, Xu JL. Thymidine kinase 1 combined with CEA, CYFRA21-1 and NSE improved its diagnostic value for lung cancer. Life Sci. 2018;194:1-6.
18. Friedl P, Alexander S. Cancer invasion and the microenvironment: plasticity and reciprocity. Cell. 2011;147:992-1009.
19. Alix-Panabières C, Pantel K. Clinical applications of circulating tumor cells and circulating tumor DNA as liquid biopsy. Cancer Discov. 2016;6:479-91.
20. Alix-Panabières C, Pantel K. Liquid biopsy: from discovery to clinical application. Cancer Discov. 2021;11:858-73.
21. Lozar T, Gersak K, Cemazar M, Kuhar CG, Jesenko T. The biology and clinical potential of circulating tumor cells. Radiol Oncol. 2024;58:458.
22. Lawrence R, Watters M, Davies CR, Pantel K, Lu YJ. Circulating tumour cells for early detection of clinically relevant cancer. Nat Rev Clin Oncol. 2023;20:487-500.
23. Brozos-Vázquez EM, Díaz-Peña R, García-González J, et al. Immunotherapy in nonsmall-cell lung cancer: current status and future prospects for liquid biopsy. Cancer Immunol Immunother. 2021;70:1177-88.
24. Krebs MG, Hou JM, Ward TH, Blackhall FH, Dive C. Circulating tumour cells: their utility in cancer management and predicting outcomes. Ther Adv Med Oncol. 2010;2:351-65.
25. Hofman V, Ilie MI, Long E, et al. Detection of circulating tumor cells as a prognostic factor in patients undergoing radical surgery for non-small-cell lung carcinoma: comparison of the efficacy of the CellSearch Assay™ and the isolation by size of epithelial tumor cell method. Int J Cancer. 2011;129:1651-60.
26. Ilie M, Hofman V, Long-Mira E, et al. Current challenges for detection of circulating tumor cells and cell-free circulating nucleic acids, and their characterization in non-small cell lung carcinoma patients. What is the best blood substrate for personalized medicine? Ann Transl Med. 2014;2:107.
27. Tanaka F, Yoneda K, Kondo N, et al. Circulating tumor cell as a diagnostic marker in primary lung cancer. Clin Cancer Res. 2009;15:6980-6.
28. Dirix L, Buys A, Oeyen S, et al. Circulating tumor cell detection: a prospective comparison between CellSearch® and RareCyte® platforms in patients with progressive metastatic breast cancer. Breast Cancer Res Treat. 2022;193:437-44.
29. Farace F, Massard C, Vimond N, et al. A direct comparison of CellSearch and ISET for circulating tumour-cell detection in patients with metastatic carcinomas. Br J Cancer. 2011;105:847-53.
30. Hillig T, Horn P, Nygaard AB, et al. In vitro detection of circulating tumor cells compared by the CytoTrack and CellSearch methods. Tumour Biol. 2015;36:4597-601.
31. Huang C, Ding S, Huang C, et al. Distribution and clinical analysis of EpCAM+/Vimentin+ circulating tumor cells in high-risk population and cancer patients. Front Oncol. 2021;11:642971.
32. Lindgren G, Wennerberg J, Ekblad L. Cell line dependent expression of EpCAM influences the detection of circulating tumor cells with CellSearch. Laryngoscope Investig Otolaryngol. 2017;2:194-8.
33. Rossi D, Dannhauser D, Nastri BM, et al. New trends in precision medicine: a pilot study of pure light scattering analysis as a useful tool for non-small cell lung cancer (NSCLC) diagnosis. J Pers Med. 2021;11:1023.
34. Keller L, Pantel K. Unravelling tumour heterogeneity by single-cell profiling of circulating tumour cells. Nat Rev Cancer. 2019;19:553-67.
35. Fiorelli A, Accardo M, Carelli E, Angioletti D, Santini M, Di Domenico M. Circulating tumor cells in diagnosing lung cancer: clinical and morphologic analysis. Ann Thorac Surg. 2015;99:1899-905.
36. Wang X, Bai L, Kong L, Guo Z. Advances in circulating tumor cells for early detection, prognosis and metastasis reduction in lung cancer. Front Oncol. 2024;14:1411731.
37. Saini VM, Oner E, Ward MP, et al. A comparative study of circulating tumor cell isolation and enumeration technologies in lung cancer. Mol Oncol. 2025;19:2014-37.
38. Thomas A, Liu SV, Subramaniam DS, Giaccone G. Refining the treatment of NSCLC according to histological and molecular subtypes. Nat Rev Clin Oncol. 2015;12:511-26.
39. He S, Liu P, Wu Y, et al. Combining rVAR2 and anti-EpCAM to increase the capture efficiency of non-small-cell lung cancer cell lines in the flow enrichment target capture Halbach (FETCH) magnetic separation system. Int J Mol Sci. 2024;25:9816.
40. Salanti A, Clausen TM, Agerbæk MØ, et al. Targeting human cancer by a glycosaminoglycan binding malaria protein. Cancer Cell. 2015;28:500-14.
41. Sun Z, Li P, Wu Z, et al. Circulating CD45+EpCAM+ cells as a diagnostic marker for early-stage primary lung cancer. Front Med Technol. 2022;4:982308.
42. Zhang Y, Men Y, Wang J, et al. Epithelial circulating tumor cells with a heterogeneous phenotype are associated with metastasis in NSCLC. J Cancer Res Clin Oncol. 2022;148:1137-46.
43. Zhang Z, Shiratsuchi H, Lin J, et al. Expansion of CTCs from early stage lung cancer patients using a microfluidic co-culture model. Oncotarget. 2014;5:12383-97.
44. Ye T, Shi H, Phan-Thien N, Lim CT, Li Y. Numerical design of a microfluidic chip for probing mechanical properties of cells. J Biomech. 2019;84:103-12.
45. Deng Z, Wu S, Wang Y, Shi D. Circulating tumor cell isolation for cancer diagnosis and prognosis. EBioMedicine. 2022;83:104237.
46. Abramson Cancer Center at Penn Medicine. The utility of circulating tumor cells as confirmation of pathologic diagnosis in patients with suspected early stage non-small cell lung cancer. 2020. Available from: https://clinicaltrials.gov/study/NCT02380196 [Last accessed on 29 Jul 2025].
47. Jin XR, Zhu LY, Qian K, et al. Circulating tumor cells in early stage lung adenocarcinoma: a case series report and literature review. Oncotarget. 2017;8:23130-41.
48. Markou AN, Londra D, Stergiopoulou D, et al. Preoperative mutational analysis of circulating tumor cells (CTCs) and plasma-cfDNA provides complementary information for early prediction of relapse: a pilot study in early-stage non-small cell lung cancer. Cancers. 2023;15:1877.
49. Wang HM, Zhang CY, Peng KC, et al. Using patient-derived organoids to predict locally advanced or metastatic lung cancer tumor response: a real-world study. Cell Rep Med. 2023;4:100911.
50. Pérez-Cabello JA, Artero-Castro A, Molina-Pinelo S. Small cell lung cancer unveiled: exploring the untapped resource of circulating tumor cells-derived organoids. Crit Rev Oncol Hematol. 2025;207:104622.
51. Lancaster MA, Knoblich JA. Organogenesis in a dish: modeling development and disease using organoid technologies. Science. 2014;345:1247125.
52. Huang L, Xu Y, Wang N, et al. Next-generation preclinical functional testing models in cancer precision medicine: CTC-derived organoids. Small Methods. 2024;8:e2301009.
53. Lin S, Huang G, Cheng L, et al. Establishment of peripheral blood mononuclear cell-derived humanized lung cancer mouse models for studying efficacy of PD-L1/PD-1 targeted immunotherapy. mAbs. 2018;10:1301-11.
54. Lahmadi M. 5P Circulating tumor cell-derived organoids from lung adenocarcinoma patients for assessment of EGFR and KRAS mutations. Ann Oncol. 2024;35:S216.
55. O'byrne KJ, Kapeleris J, Kulasinghe A, et al. Culture of circulating tumour cells derived from non-small cell lung cancer. JCO. 2020;38:e21692.
56. De Renzi G, de Marco G, de Meo M, Del Rosso E, Gazzaniga P, Nicolazzo C. In vitro cultures of circulating tumor cells: a potential tool to unravel drug sensitivity. Cancer Drug Resist. 2022;5:245-60.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Copyright
Data & Comments
Data


















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at [email protected].