Volume 5, Issue 1 (2024) – 11 articles
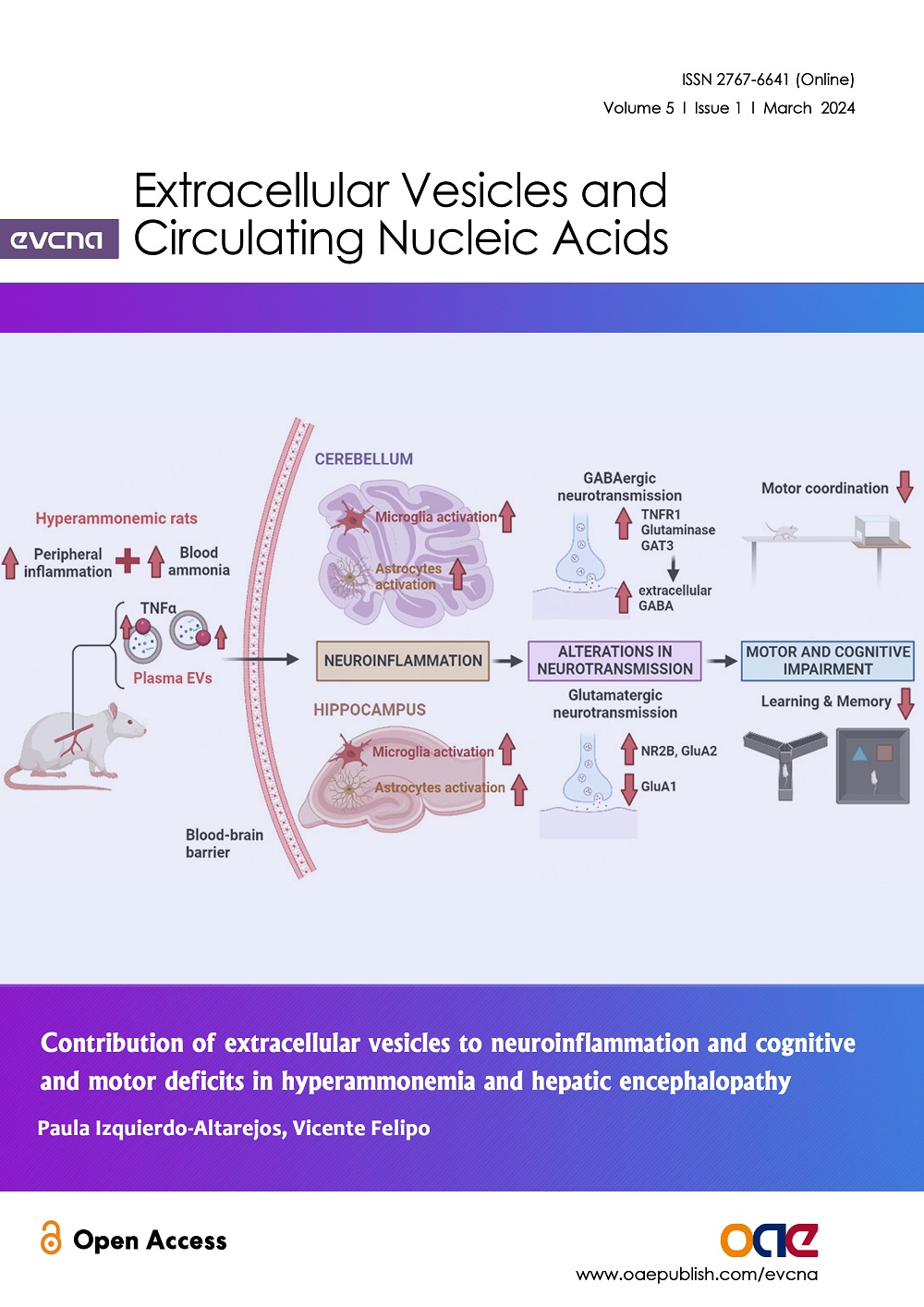
Cover Picture: Hepatic encephalopathy (HE) is a neuropsychiatric disorder that can affect cirrhotic patients. Hyperammonemic (HA) rats are a stablished model of this pathology and reproduce the motor and cognitive deficits shown in patients. HE is characterized by hyperammonemia and peripheral inflammation, which lead to neuroinflammation, alterations in the neurotransmission and, ultimately, to the motor and cognitive impairment. Plasmatic extracellular vesicles (EVs) are a recently discovered communication mechanism between the periphery and the brain. The quantity of EVs is elevated in plasma of HA rats and they contain higher levels of the proinflammatory cytokine TNFα. These EVs can cross the blood-brain-barrier, reaching two key areas: cerebellum and hippocampus. HA-EVs induce neuroinflammation, activating microglia and astrocytes and this leads to alterations in neurotransmission. In cerebellum, GABAergic neurotransmission is altered, including an activation of the TNFR1-glutaminase-GAT3 pathway, which increases extracellular GABA levels, leading to the motor incoordination observed. In hippocampus, alterations affect mainly glutamatergic neurotransmission, changing the membrane expression of AMPA (NR2B subunit) and NMDA receptors (GluA1 and GluA2 subunits), which leads to learning and memory impairment. Understanding the implication of the EVs in the pathology development would be helpful to identify potential diagnostic and therapeutic targets for patients with HE.
view this paper