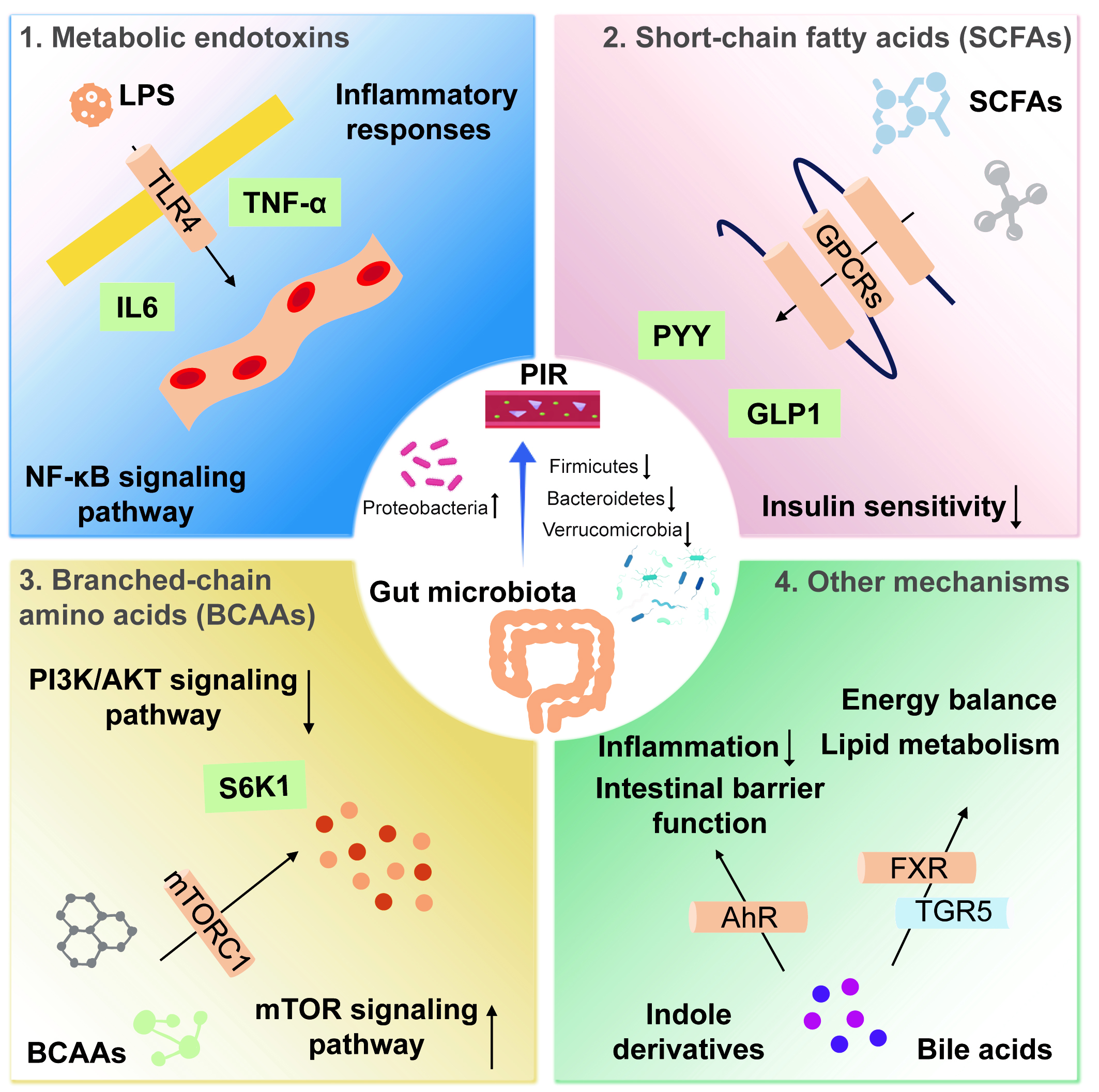
fig1
Figure 1. Mechanisms by which the gut microbiota influences postoperative insulin resistance. (1) LPS is a potent inflammatory mediator that binds to TLR4, activating the NF-κB signaling pathway and inducing the release of inflammatory cytokines, such as TNF-α and IL-6; (2) SCFAs act via GPCRs, whose activation promotes the secretion of GLP-1 and PYY; (3) BCAAs impair insulin signaling by inhibiting the PI3K/AKT pathway through activation of the mTORC1. mTORC1 activation induces phosphorylation of downstream S6K1; (4) Bile acids enhance insulin sensitivity by activating receptors such as the FXR and TGR5. Indole derivatives regulate host inflammation and metabolic health by activating the AhR. AhR activation alleviates inflammation, improves intestinal barrier function, and may enhance insulin sensitivity by modulating metabolic pathways. LPS: Lipopolysaccharide; TLR4: Toll-like receptor 4; NF-κB: nuclear factor-κB; TNF-α: Tumor necrosis factor-α; IL-6: interleukin-6; SCFA: short-chain fatty acid; GPCR: G protein-coupled receptor; GLP-1: glucagon-like peptide-1; PYY: peptide YY; BCAA: branched-chain amino acid; mTORC1: mammalian target of rapamycin complex 1; PI3K: phosphatidylinositol 3-kinase; protein kinase B; FXR: farnesoid X receptor; TGR5: G protein-coupled receptor 5; AhR: aryl hydrocarbon receptor; PIR: postoperative insulin resistance.