Simultaneous robotic liver resection and left colectomy for sigmoid colon cancer with synchronous liver metastases using the same robotic trocar positioning
Abstract
Watch a video of this article.
BRIEF EXPLANATION
Colorectal cancer (CRC) remains one of the most common cancers[1]. Despite advances in understanding its pathogenetic mechanisms, metastatic CRC continues to pose a major clinical challenge, with colorectal liver metastasis (CRLM) being the critical cause of CRC-related death due to limited therapeutic options and poor prognosis[2]. Liver resection remains the only potentially curative treatment for patients with CRLM[3]. Three approaches to treating CRC with liver metastases have been proposed, all preceded by neoadjuvant chemotherapy (nCT)[4]: colonic resection followed by adjuvant chemotherapy (aCT) and then liver resection; hepatic resection followed by aCT and then colonic resection; or simultaneous colonic and hepatic resection followed by aCT. For patients with unresectable CRLM, palliative chemotherapy is the only option, with a 5-year overall survival rate of only 10%[3].
In recent years, simultaneous robotic resections have been increasingly adopted for properly selected patients[5], due to the enhanced maneuverability provided by robotic platforms. The presented video [Video 1] demonstrates a single-docking robotic left colectomy combined with ultrasound-guided, parenchymal-sparing wedge resection of liver segments 7 and 8, and left hemicolectomy with mechanical anastomosis according to the Knight-Griffen technique. This procedure was performed on a patient with sigmoid cancer and a solitary liver metastasis following four cycles of neoadjuvant FOLFOX chemotherapy.
The port placement strategy and key surgical steps are shown in Figures 1-4. The total operative time was 320 min, with an estimated blood loss of 100 cc. Postoperatively, the patient reported a pain score of 3 on the Numerical Rating Scale (NRS) on day 1, which decreased to 1 on day 2 and 0 on day 3. Bowel movements were observed on postoperative day (POD) 0, with flatus on POD 1, allowing for initiation of solid oral intake that evening. The first evacuation of solid stools occurred on POD 3. Following a follow-up abdominal ultrasound, the patient was discharged on POD 5.
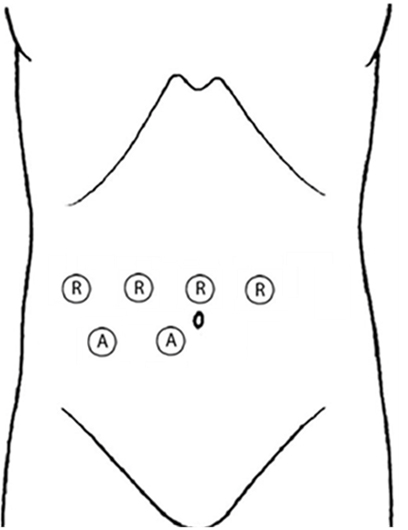
Figure 1. Port placement for liver wedge resection and splenic flexure mobilization. R: Robotic trocar; A: Assistant laparoscopic trocar.
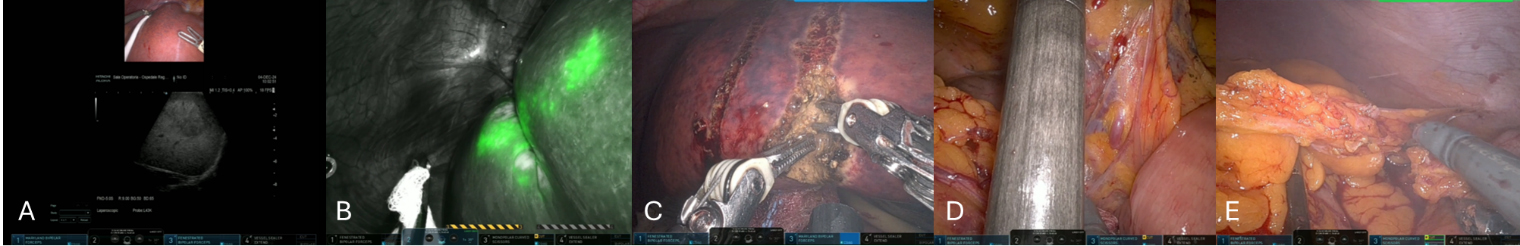
Figure 2. Key surgical steps performed using the trocar configuration shown in Figure 1. (A) Intraoperative ultrasonography; (B) Identification with indocyanine green; (C) Liver transection using the MAMBA technique; (D) Inferior mesenteric artery and vein identification; (E) Splenic flexure mobilization.
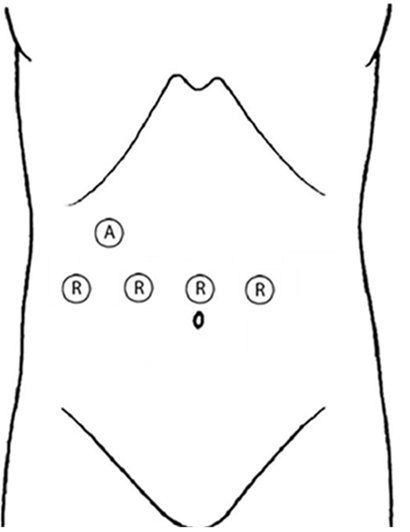
Figure 3. Port placement for the remaining left colectomy. R: Robotic trocar; A: Assistant laparoscopic trocar.
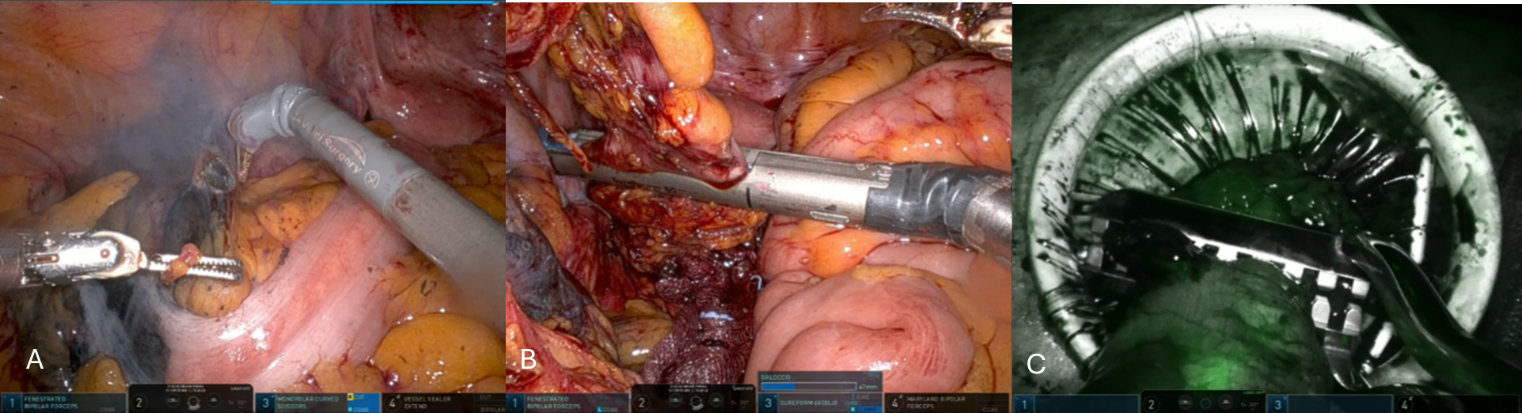
Figure 4. Key surgical steps performed using the trocar configuration shown in Figure 3. (A) Left paracolic gutter dissection; (B) Distal bowel transection with robotic stapler; (C) Extracorporeal proximal bowel transection with perfusion assessment using Indocyanine green.
Histologic examination revealed pT3N0M1a according to the AJCC 8th edition. The patient has completed six of the planned eight cycles of adjuvant FOLFOX chemotherapy, and at the 6-month follow-up visit, she was in excellent general condition, with a negative CT scan for disease recurrence.
By carefully positioning the da Vinci Xi robot ports, this synchronous surgery can be performed without altering the original robotic trocar configuration, with the addition of only an assistant trocar. Thanks to the articulated design of the robotic system, such complex operations can be safely performed across two distinct abdominal regions while maintaining the advantages of minimally invasive surgery, including shorter hospital stays, reduced morbidity, and lower blood loss.
DECLARATIONS
Authors’ contributions
Creation of manuscript: Caringi S, Madaro A, Memeo R
Video creation: Caringi S
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
This video article did not require ethics committee approval. The patient signed an informed consent form.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2025.
Supplementary Materials
Please note: The publisher is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing content) should be directed to the corresponding author for the article.
REFERENCES
1. World Health Organization News Page. Available from: https://www.who.int/news/item/01-02-2024-global-cancer-burden-growing--amidst-mounting-need-for-services (Accessed on 2025-8-14).
2. Cañellas-Socias A, Sancho E, Batlle E. Mechanisms of metastatic colorectal cancer. Nat Rev Gastroenterol Hepatol. 2024;21:609-25.
3. Adam R, de Gramont A, Figueras J, et al; of the EGOSLIM (Expert Group on OncoSurgery management of LIver Metastases) group. Managing synchronous liver metastases from colorectal cancer: a multidisciplinary international consensus. Cancer Treat Rev. 2015;41:729-41.
4. Van Cutsem E, Cervantes A, Adam R, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol. 2016;27:1386-422.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Special Issue
Copyright
Data & Comments
Data
















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at [email protected].