Advances in the application of artificial intelligence in continuing education for trauma orthopedics
Abstract
The application of artificial intelligence (AI) in continuing education for traumatic orthopedics is rapidly evolving and demonstrates significant potential. Through AI technologies, surgeons can enhance their surgical skills and operational confidence within safe simulated environments, particularly in contexts where hands-on practice opportunities are diminishing. However, the long-term efficacy of AI in continuing education remains incompletely validated, with further research required to assess skill retention among trainees and the practical outcomes of its application. Additionally, AI holds substantial promise in clinical diagnosis and decision-making support, enabling surgeons to rapidly analyze and process complex data in trauma and emergency settings. Despite its broad prospects in acute surgical interventions and educational training, the adoption of AI remains in its nascent stage due to limited physician understanding of AI technologies and current technical constraints. AI also exhibits advantages in personalized teaching by assessing trainee competencies and providing feedback to optimize educational processes. Nevertheless, challenges such as data imbalance and insufficient sample sizes persist in AI-driven continuing education. While the widespread integration of AI in orthopedic trauma education - particularly in medical imaging diagnostics and surgical training - can significantly improve clinical outcomes, physicians must fully acknowledge its limitations and exercise prudence when implementing AI solutions.
Keywords
INTRODUCTION
In recent years, the fields of continuing medical education and clinical practice within trauma orthopedics have undergone significant transformations, largely driven by rapid advancements in technology, particularly artificial intelligence (AI). Continuing education in trauma orthopedics has notably benefited from innovations in simulation-based training, cost-effective educational programs, and digital integration, collectively contributing to enhanced skill acquisition, reduced clinical risks, and improved training accessibility. Simulation-based training has provided trainees with safe, controlled environments to refine operative skills, boosting their confidence and procedural competence. Meanwhile, cost-effective curricula have expanded access to essential surgical skills training, particularly in resource-limited regions, although standardized assessment frameworks still require further development.
The integration of digital learning tools and AI-driven systems into orthopedic education has opened new avenues for personalized, efficient learning experiences. AI applications, including robotic-assisted surgeries, diagnostic imaging enhancements, predictive modeling, and virtual reality (VR) simulations, have demonstrated significant potential in optimizing surgical outcomes and decision-making processes. However, these technological advances also pose notable challenges, including data availability, algorithm transparency, ethical considerations, and the need for rigorous validation of long-term clinical efficacy.
Despite these hurdles, the potential of AI and digital technologies to revolutionize orthopedic trauma education and clinical practice is profound. Addressing existing gaps through standardized evaluations, comprehensive competency assessments, and careful management of AI integration into clinical workflows will be critical for sustaining and enhancing educational quality and patient care outcomes in trauma orthopedics.
In this work, a systematic literature review was conducted using databases such as PubMed, Google Scholar, and Web of Science. The search focused on articles published from 2010 to 2025 with the keywords ‘AI in trauma orthopedics’, ‘artificial intelligence in medical education’, and ‘AI diagnostic tools’. Studies published in English in peer-reviewed journals were included. Articles focusing on general AI applications in medicine, outside the context of trauma orthopedics, were excluded.
TECHNOLOGICAL ADVANCEMENTS IN CONTINUING MEDICAL EDUCATION FOR TRAUMA ORTHOPEDICS
Simulation-based training in trauma orthopedics
In recent years, technological advancements in continuing medical education for trauma orthopedics have primarily focused on three areas: simulation-based training, cost-effective curricula, and digital tool integration. Simulation technology has emerged as a pivotal component of orthopedic trauma training, providing learners with risk-free environments to enhance procedural competence and confidence while minimizing patient risk. Stirling’s study demonstrated that high-fidelity simulation training improved trainees’ surgical skill acquisition efficiency by 40%, particularly in mastering operative techniques. Notably, AI-powered VR systems achieved 92% fidelity in complex fracture reduction simulations, although this necessitates establishing multicenter training databases. Aviation industry-inspired competency maintenance models propose progressively increasing simulation duration from the current 30% to 60% of training time, incorporating non-technical skill modules, such as decision-tree analysis. Current evidence indicates a 41% reduction in complication rates during initial independent tibial intramedullary nailing procedures among simulation-trained residents, substantiating the “simulation-to-clinical” competency transfer model. However, long-term skill retention and validation of sustained efficacy require further investigation[1].
Mackenzie et al. systematically evaluated trauma surgical skill programs, revealing that flagship courses including Advanced Trauma Life Support (ATLS), Advanced Surgical Skills for Exposure in Trauma (ASSET), and Advanced Trauma Operative Management (ATOM) significantly enhanced open surgical competencies through cadaveric labs and modular curricula. Specifically, ATLS-standardized protocols improved decision-making speed by 30%, while ASSET increased anatomical exposure success rates from a baseline of 65% to 92%. Nevertheless, these improvements remain confined to controlled simulated environments, with clinical applicability yet to be quantified. The Kirkpatrick evaluation model currently reaches only Levels 2-3 (knowledge retention and behavioral changes), lacking standardized metrics for longitudinal monitoring of skill maintenance[2,3]. Research by Moran and George corroborates the efficacy of simulation training in enhancing novices’ clinical judgment, although longitudinal outcome data remain insufficient[4].
Cost-optimized training paradigms
Cost-optimized training paradigms have gained traction in addressing reduced operating room opportunities. Davies et al.[5] developed a budget-conscious curriculum featuring dry bone workshops with a 1:4 instructor-student ratio and industry-sponsored hands-on sessions, achieving 95%-100% satisfaction rates at a cost of £50 per participant. Curriculum iterations showed significant improvements: the 2008 cohort’s informal lectures (P = 0.044 satisfaction variance) were replaced by practical modules, with 2009 data demonstrating enhanced intramedullary nailing instruction quality. However, the evaluation relied solely on Likert-scale subjective assessments rather than objective metrics such as the Objective Structured Assessment of Technical Skills (OSATS), with insufficient two-year follow-up for long-term efficacy validation. While subjective metrics, such as Likert-scale surveys, are commonly used to assess learner satisfaction, it is crucial to incorporate objective measures such as OSATS scores and longitudinal data to assess skill retention and the real-world impact of AI technologies on surgical competencies.
Digital transformation in orthopedic education
Digital transformation is reshaping the infrastructure of orthopedic education. Suárez et al.[6] emphasized the growing role of virtual learning resources, advocating for the expanded development of adaptive digital platforms. The Orthopaedic Trauma Association (OTA) provides comprehensive online resources, although Mehta and Smith[7] note limited evidence regarding their longitudinal impacts. Globally, particularly in low-income regions, continuing medical education serves as a critical conduit for the dissemination of surgical skills.
In conclusion, while simulation technologies, cost-effective curricula, and digital innovations have substantially advanced trauma orthopedic training, future research must prioritize: (1) Standardized outcome measurement frameworks integrating OSATS and clinical endpoints; (2) Longitudinal competency retention studies establishing recertification intervals; and (3) Rigorous evaluation of digital resource efficacy. Addressing these gaps will ensure sustainable improvements in the quality of postgraduate orthopedic education.
APPLICATIONS OF ARTIFICIAL INTELLIGENCE IN TRAUMA ORTHOPEDICS
AI applications and potential in trauma orthopedics
Against the backdrop of rapidly advancing medical technology, the widespread application of AI and Machine Learning (ML) in the field of trauma orthopedics has sparked growing academic discussion and research interest. With the evolution of technology and increased data availability, studies utilizing AI and ML in trauma orthopedics have steadily increased, covering key aspects such as imaging diagnostics, disease classification, treatment recommendations, and postoperative rehabilitation management. Systematic reviews have shown that AI holds tremendous potential in orthopedic surgery, particularly in early disease detection, surgical planning optimization, and postoperative complication risk prediction. The introduction of such technologies not only improves diagnostic accuracy but also aids physicians in developing more scientific and personalized treatment strategies through intelligent risk assessment models, thereby significantly enhancing patient outcomes and surgical success rates[8,9].
Advantages, challenges, and clinical integration barriers
An increasing number of surgeons have pointed out that AI technologies offer clear advantages in managing severe trauma cases and urgent medical decision making. Especially in time-critical situations with limited information, AI-assisted systems can process large volumes of clinical data rapidly, providing real-time analysis and decision support, thereby greatly enhancing a surgeon’s judgment and responsiveness. However, despite these promising prospects, the widespread clinical adoption of AI technologies still faces numerous technical and practical challenges. These include insufficient algorithm interpretability, inconsistent data standards, limited model generalizability, and unresolved ethical and privacy concerns - all of which are key factors hindering broader implementation. Therefore, future development should focus on addressing these bottlenecks to improve the practicality and reliability of AI technologies[10,11].
Empirical studies further indicate that while clinicians generally recognize the transformative potential of AI in enhancing healthcare quality and efficiency, its integration into actual medical practice remains limited. This is mainly due to two factors: first, many medical professionals lack sufficient knowledge of AI technologies due to insufficient systematic training and education; second, AI tools often have poor compatibility with existing clinical workflows and equipment systems, leading to inconvenience or steep learning curves in real-world applications, which hampers their adoption and effectiveness[12,13].
Robotic-assisted surgery and diagnostic support
In trauma orthopedic surgery, robotic-assisted surgical systems - one of the key applications of AI - have made significant progress in recent years. These systems, equipped with precise navigation and real-time feedback mechanisms, enable more accurate and stable surgical operations, particularly in minimally invasive procedures. Surgical robots not only enhance precision and shorten operating time but also reduce tissue damage and postoperative complications, thereby improving patients’ recovery experiences and overall treatment outcomes[14]. However, the application of such technologies is still largely limited to high-end medical institutions. Their high costs and complex maintenance requirements have prevented widespread adoption in most grassroots hospitals. Hence, there is an urgent need for more multicenter, long-term clinical studies to verify their broad applicability and long-term benefits, thereby promoting their adoption across different levels of the healthcare system[15].
Moreover, the clinical value of AI extends far beyond surgical operations, showing great promise in diagnostic processes as well. For instance, in fracture detection and assessment, deep learning-based neural network models have been shown to significantly enhance the accuracy of medical image interpretation. This is particularly valuable when radiologists are inexperienced or when cases are complex. Trained on large-scale imaging datasets, these models can automatically identify fracture types, locate injury sites, and even predict risk levels, thus assisting doctors in making more comprehensive and accurate diagnostic decisions[16].
Future directions: personalized medicine and implementation strategies
Despite the powerful technical potential and application prospects of AI in trauma orthopedics, its deployment in real-world clinical settings must proceed with caution. Numerous studies have confirmed that AI improves imaging diagnostic efficiency and facilitates surgical training; however, before it can be officially integrated into clinical decision making, its safety, efficacy, interpretability, and ethical risks must be thoroughly assessed. In particular, there is a pressing need to establish strict regulatory frameworks and standardized guidelines for patient data protection and to mitigate algorithmic bias. To successfully integrate AI tools into clinical workflows, hospitals and educational institutions should prioritize AI solutions based on cost-effectiveness and compatibility with existing systems. Practical AI solutions that address educational gaps, such as in surgical skill development in low-resource regions, should be implemented first.
It is also worth noting that the advantages AI demonstrates in personalized medicine and surgical path planning are gradually transforming traditional medical practice. By analyzing multimodal medical data - including patient history, lab results, and imaging data - AI can provide evidence-based personalized treatment suggestions, enabling more precise patient management and decision making[17]. Looking ahead, future research should place greater emphasis on validating AI systems across diverse populations and clinical scenarios, continuously driving the transition from laboratory innovation to clinical implementation. Ultimately, this will realize the full integration of AI in trauma orthopedics and usher in a new era of intelligent orthopedic care.
APPLICATION OF ARTIFICIAL INTELLIGENCE IN CONTINUING EDUCATION IN TRAUMA ORTHOPEDICS
The emerging role of AI in trauma orthopedic education
In recent years, the rapid development of AI in the medical field has brought about unprecedented transformation and opportunities in continuing medical education, particularly in trauma orthopedics. As a cutting-edge technology, AI has demonstrated significant potential not only in supporting clinical diagnosis, optimizing treatment plans, and predicting prognoses, but also in advancing medical education. With the ever-expanding and rapidly evolving body of medical knowledge, traditional teaching methods often fall short in meeting the growing demands for efficient learning and accurate skill acquisition among healthcare professionals. The integration of AI technologies offers promising solutions to address these challenges.
Numerous studies have shown that both medical students and practicing clinicians generally support incorporating AI into the medical education system, recognizing its substantial educational value. On the one hand, AI can enhance clinical decision making by leveraging data-driven models; on the other hand, it boosts teaching efficiency and quality through applications in medical image analysis, case-based learning, and personalized content delivery. For instance, a study by Civaner et al. revealed that while the clinical applications of AI tools are becoming increasingly widespread, medical students also express concerns - particularly regarding the potential impact of AI on the trust between physicians and patients and professional ethical obligations. This highlights the necessity of concurrently developing ethical frameworks and fostering trust while promoting the adoption of AI in educational settings[18].
Global demand and practical advantages of AI education
In addition, the demand for AI-related education is unevenly distributed across the globe. A global mixed-methods study reported that students in low- and middle-income countries are especially eager to receive training in fundamental AI technologies, to support local healthcare innovation[19]. Meanwhile, Boillat et al. found, through a questionnaire-based study, that although the current understanding of AI among students and clinicians is limited, most believe that continuing medical education is essential to enhancing their knowledge and practical skills in this area[20]. This further underscores the urgency of integrating AI education into medical training.
In practical applications, AI offers numerous advantages. Through deep learning and big data algorithms, AI can significantly enhance the accuracy of preoperative assessments, intraoperative navigation, postoperative rehabilitation monitoring, and complication prediction in trauma orthopedics[21]. These capabilities not only reduce physicians’ workload but also facilitate the implementation of personalized medicine and precision teaching. For example, AI systems can analyze a physician’s clinical decision patterns to recommend relevant learning content or simulate case scenarios, helping learners acquire critical knowledge and skills in a more targeted and time-efficient manner.
Implementation challenges and curriculum design
Nevertheless, the implementation of AI in continuing medical education is not without challenges. Busch et al. emphasized the urgent need for medical education institutions to establish comprehensive ethical guidelines to ensure the safe and compliant use of AI technologies[22]. These guidelines must address data privacy, security, algorithmic transparency, and the balance between AI systems and human judgment. For instance, while AI can provide rapid decision support during clinical training, its “black box” nature may impede learners’ understanding of the diagnostic reasoning process and reduce their confidence in making independent clinical judgments.
Regarding curriculum design, Krive et al. argued that AI education should go beyond theoretical instruction and focus on practical, real-world applicability. Courses should emphasize hands-on learning through simulations, interactive platforms, and case-based teaching to ensure that learners can effectively operate AI tools and understand their roles and limitations in clinical decision making[23].
As educational technologies evolve, the use of AI in trauma orthopedic education is expanding. By integrating AI with VR or augmented reality (AR), realistic surgical simulation environments can be created, allowing students and clinicians to practice procedures in a risk-free setting. This enhances not only technical proficiency but also comprehension of complex anatomical structures and workflows[24,25]. Additionally, AI-powered learning platforms can track learners’ progress and performance, offering personalized learning pathways and thereby realizing a more tailored and effective education model.
Limitations, ethical considerations, and future directions
Moreover, although AI tools can provide immediate clinical advice in certain settings, their diagnostic and decision-making accuracy still requires significant improvement. For instance, Boddu et al. reported that during intensive care unit (ICU) ward rounds, AI tools were able to generate real-time suggestions, but their accuracy was often inferior to that of experienced human physicians, underscoring the need for cautious use of AI in critical clinical contexts[26]. Indeed, while AI has demonstrated relatively high accuracy in imaging diagnostics, its performance in more complex environments, such as ICU care, remains inconsistent. This discrepancy may be explained by differences in clinical data quality, the complexity of trauma cases, and the specific application context. For example, imaging diagnostics usually benefit from high-quality and standardized datasets, whereas ICU environments frequently require real-time decision making under conditions of limited or incomplete data, which constrains the effectiveness of AI.
From a broader perspective, the widespread adoption of AI in continuing medical education requires overcoming both technical and ethical barriers. Scholars such as Wartman and Combs have noted that AI can effectively alleviate physicians’ information overload and improve their collaboration with AI systems. However, to achieve this goal, medical education must strengthen knowledge management systems and offer comprehensive AI training programs[27,28]. These programs should not only focus on technical skills but also include instruction on applying AI in real-world clinical decision-making scenarios.
In conclusion, AI presents a transformative opportunity for continuing education in trauma orthopedics. It enhances the efficiency and quality of education, providing clinicians with more precise and individualized learning paths. However, its introduction also brings a range of challenges - technical, ethical, and structural - that require coordinated efforts among educators, developers, and policymakers. A scientifically grounded, ethically sound, and practically oriented educational framework must be established to ensure the responsible development and integration of AI in medical education, ultimately driving innovation in physician training and improving patient-care outcomes.
CLINICAL EFFECTIVENESS AND CHALLENGES OF ARTIFICIAL INTELLIGENCE IN CONTINUING EDUCATION IN TRAUMA ORTHOPEDICS
AI in surgical training
The rapid development of AI technology is gradually transforming continuing education and clinical practice in the field of trauma orthopedics, particularly demonstrating significant potential in surgical training and clinical decision making. During surgeons’ training, AI-driven simulation training systems play a crucial role. These systems allow physicians to undertake operational training in highly realistic and controlled environments. Particularly when actual clinical surgical opportunities are limited, simulation systems can provide more frequent “hands-on practice” opportunities. This virtual training not only effectively enhances trainees’ surgical skills but also boosts their confidence and proficiency in complex surgical scenarios, while reducing uncertainties and risks associated with a lack of practical experience[29].
AI as a clinical decision support tool
In terms of clinical decision support, AI has demonstrated exceptional potential. It can analyze vast datasets and provide accurate recommendations, assisting surgeons in making more informed decisions in emergency situations. This is particularly important for trauma orthopedic surgeons, who frequently face urgent surgical timelines and complex case management requirements. However, despite AI’s powerful data analysis and predictive capabilities, many physicians remain cautious about its practical application in clinical decision making. They believe that AI technology is still in its early stages of development and requires further research and continuous training programs to ensure its effectiveness and reliability in clinical practice[30].
Relevant studies further support this viewpoint, indicating that most trauma and emergency surgeons recognize AI’s auxiliary role in acute surgeries. Especially when dealing with complex surgical procedures, AI can help physicians quickly analyze and process large amounts of patient data. However, the application of AI in trauma orthopedics is still in its early stages, and its true potential remains to be explored and utilized further[31]. Nonetheless, AI has already demonstrated unique advantages in surgical education. For instance, it can optimize the assessment and classification of trainees’ skills. Through precise data analysis, AI systems provide personalized feedback to trainees, effectively enhancing learning outcomes and operational proficiency. This real-time feedback mechanism helps trainees identify their shortcomings and guides instructors in improving teaching methods, further enhancing educational effectiveness[32].
AI in educational assessment and personalized feedback
AI holds significant potential in advancing continuing education and clinical practice in trauma orthopedics, particularly in resource-limited settings, where it may help mitigate global health disparities. Nevertheless, its integration still faces several challenges[33]. First, data imbalance and insufficient sample sizes limit the widespread application of AI models. In trauma orthopedics, particularly in emergency scenarios, it is often difficult to obtain sufficient high-quality data to train robust and reliable models[34,35]. In addition, the interpretability and transparency of AI remain key technical bottlenecks, as clinicians generally expect to understand the rationale behind AI-driven decisions to better integrate them into clinical practice[36,37]. Ethical concerns, such as algorithmic bias and data fairness, must also be addressed carefully to ensure that AI reduces rather than exacerbates healthcare inequalities[38]. Further research should focus on the role of AI in promoting global health equity, particularly in under-resourced regions[39]. Meanwhile, trauma consultation meetings, as an essential component of orthopedic training, provide trainees with opportunities to directly engage in case discussions and gain deeper insights into complex case management. However, feedback from trainees suggests that time constraints and insufficient learning environments may hinder the effectiveness of such consultations, indicating that their structure requires further optimization[40,41]. In the future, integrating AI with traditional educational modalities may help maximize its value in trauma orthopedic continuing education[42].
Challenges and future directions in trauma orthopedic AI applications
Despite these challenges, the prospects for AI applications in trauma orthopedics remain broad. Particularly in areas such as fracture image recognition and complex surgical decision support, AI technology has demonstrated immense potential. AI systems can rapidly and accurately analyze X-rays or computed tomography (CT) images through automated image recognition technology, assisting physicians in the earlier and more accurate identification of fracture types and severity. Additionally, AI can integrate medical history data, preoperative assessment results, and other information to generate predictive models for postoperative complications, providing surgeons with personalized postoperative management recommendations, thereby further improving patient prognosis[43].
THE PROSPECTS OF ARTIFICIAL INTELLIGENCE TECHNOLOGY IN THE FIELD OF ORTHOPEDIC TRAUMA SURGERY
Simulation-based and low-cost training in orthopedic trauma education
In recent years, continuing education in orthopedic trauma surgery has witnessed significant advancements, particularly in simulation training, low-cost courses, and digital tool applications. For instance, simulation training provides trainees with a safe and efficient operational environment, significantly enhancing surgical skill acquisition; however, studies on long-term skill retention and effectiveness evaluation remain insufficient[44]. Although simulation technology has been shown to improve surgeons’ confidence and skill levels in complex procedures, its long-term efficacy in actual clinical practice requires further research[45] [Table 1].
Summary of technological advancements, achievements, challenges, and future directions in trauma orthopedic continuing education and clinical application
| Domain | Key advances | Achievements | Challenges | Future directions | Basis & key refs. |
| Simulation-based training | High-fidelity simulation systems; AI-powered VR simulation environments | 40% improvement in surgical skill acquisition efficiency; 41% reduction in initial complication rates | Unclear long-term skill retention; lack of multicenter training databases | Standardize evaluation frameworks (e.g., OSATS); conduct longitudinal competency retention studies | Multiple reviews & pre- and post-benchmark studies support simulation efficacy for skills and safety; long-term and multicenter RCTs remain scarce. [1-3,27,34] |
| Cost-effective curricula | Low-cost dry bone workshops; industry-sponsored hands-on sessions | 95%-100% satisfaction rates; significant improvement in teaching quality for intramedullary nailing | Reliance on subjective assessments; insufficient two-year follow-up data | Integrate objective assessment tools; expand access to affordable and practical training programs | Evidence mainly from single-center observational reports with satisfaction outcomes; objective, long-term endpoints are limited. [4,35] |
| Digital tool integration | Adaptive online learning platforms; virtual resource expansion | Improved accessibility and flexibility of continuing education | Limited evidence of sustained long-term effectiveness; implementation sustainability issues | Establish comprehensive outcome measurement systems for digital education | Predominantly scoping reviews, perspectives, and early evaluations in surgery/medical education; durability data are limited. [26,30,33] |
| AI applications in trauma orthopedics | Imaging diagnostics; surgical planning optimization; postoperative risk prediction; robotic-assisted surgery | Enhanced diagnostic accuracy; improved surgical precision; better patient outcomes | Insufficient algorithm interpretability; data standardization issues; ethical and privacy concerns | Enhance algorithm transparency; develop universal clinical validation standards | Mix of reviews, protocols, and narrative guidance; strong signals in imaging/robotics precision, but fewer high-quality outcome trials in trauma orthopedics. [7,10,12-15,28,29,31,32] |
| AI in continuing medical education | Personalized adaptive learning; AI-driven case simulations; real-time skill assessment | Increased efficiency and precision of learning; targeted knowledge acquisition | Risk of reduced physician-patient communication skills; ethical concerns regarding AI in education | Develop AI education curricula incorporating ethical training; maintain balance between AI and human interaction | Evidence from needs assessments, mixed-methods surveys, pilot uses in education; few controlled learning-outcome trials. [16-24,30] |
| Clinical effectiveness of AI | Decision support systems; automated imaging analysis; predictive modeling of surgical outcomes | Accelerated data processing; improved emergency trauma decision making | Data imbalance; limited interpretability of AI decisions | Collect larger, diverse datasets; improve model explainability; optimize integration into clinical workflows | Early decision-support & predictive models; clinician surveys; authoritative perspectives highlight promise but limited prospective, multicenter validation. [8-10,25,28,31,32] |
| Prospects in orthopedic trauma surgery | Simulation training; low-cost curriculum development; digital and AI integration | Enhanced clinical outcomes; support for global education initiatives | High cost and complexity limit broad adoption; lack of long-term clinical outcome studies | Promote multicenter, long-term validation research; foster affordable and scalable AI solutions | Largely narrative/synthesis and platform overviews; real-world, long-horizon outcome evidence is still emerging. [3,11,12,28-30,33] |
Table 1 summarizes the major domains discussed regarding the integration of technology and AI into trauma orthopedic continuing education and clinical practice. Key advances, achievements, challenges, and proposed future directions are outlined to guide future research and development efforts.
Regarding low-cost training courses, particularly in resource-limited countries and regions, their widespread implementation has provided valuable support for orthopedic trauma education. However, quantitative assessments of these programs need further refinement[46]. Relevant studies suggest that low-cost practical courses can significantly enhance trainee satisfaction and help learners acquire essential skills despite limited opportunities for hands-on experience in operating rooms[47].
Digital resources and online learning tools
The integration of digital resources and online learning tools has opened new avenues for continuing education in orthopedic trauma. Research indicates that digital educational resources not only support autonomous learning but also improve teaching effectiveness, although their long-term application efficacy still requires further evaluation[48]. For example, the OTA provides practitioners with extensive online learning resources, yet how to more effectively implement these resources and ensure their sustainability remains an urgent issue[49].
Artificial intelligence in education and clinical practice
The extensive application of AI technology, including imaging diagnostics and predictive tools, has further driven advancements in orthopedic trauma education. While AI holds great potential to improve clinical outcomes, medical professionals must adopt these technologies cautiously, ensuring a comprehensive understanding of their limitations[50]. Research indicates that digital educational resources not only support autonomous learning but also improve teaching effectiveness, although their long-term application efficacy still requires further evaluation. To facilitate a clearer understanding, Table 2 provides a comparative summary of three representative approaches - simulation-based training, cost-effective curricula, and digital/AI-enhanced education - across five key dimensions (efficiency, accessibility, personalization, long-term effectiveness, and ethics/transparency). This comparative perspective highlights how these different methods complement each other, offering practical guidance for optimizing future trauma orthopedic education strategies.
Comparative summary of three major approaches in continuing education for trauma orthopedics: simulation-based training, cost-effective curricula, and digital/AI-enhanced education
| Dimension | Simulation-based training | Cost-effective curricula | Digital/AI-enhanced education |
| Efficiency | Improves skill acquisition efficiency (↑40%), shortens learning curve | Limited efficiency, more dependent on learner initiative | Significantly improves efficiency, supports rapid data processing and precision teaching |
| Accessibility | Moderate, requires costly equipment and facilities | High, widely applicable in resource-limited settings | Moderate, advanced AI/VR tools remain expensive |
| Personalization potential | Low, mostly relies on standardized curricula | Low, lacks personalized pathways | High, adaptive systems can tailor learning based on learner performance |
| Long-term effectiveness | Limited evidence, retention requires further validation | Lacks long-term follow-up, uncertain sustained effect | Promising, but requires multicenter and long-term validation |
| Ethics/transparency | Low risk, methods transparent | Low risk, minimal ethical concerns | Challenged by algorithm ‘black- box’, data privacy, and reduced human interaction |
Overall, the broad implementation of AI technologies in orthopedic trauma surgery - covering imaging diagnostics, predictive tools, and innovative surgical training - demonstrates significant potential to enhance clinical outcomes[51,52]. Nonetheless, medical professionals should fully recognize the limitations associated with these technologies and implement them cautiously in practice[53,54]. With ongoing advancements in AI technology and its deepening integration into medical fields, AI is expected to play an increasingly pivotal role in future orthopedic trauma continuing education and clinical practice, continuously driving improvements in healthcare outcomes[55].
AI ETHICS AND GLOBAL HEALTH EQUITY IN TRAUMA ORTHOPEDIC EDUCATION
AI ethics linkages
The integration of AI into trauma orthopedic continuing education and clinical practice raises pressing ethical considerations. While AI-driven tools can enhance diagnostic accuracy, personalize learning, and accelerate decision making, their reliance on large datasets and complex algorithms inevitably introduces challenges of transparency, accountability, and trust[53,54]. The so-called “black-box” nature of many AI models can undermine physicians’ confidence in understanding and validating AI-generated outputs, potentially leading to over-reliance or misinterpretation[51]. Moreover, issues of data privacy and patient confidentiality are particularly salient, as medical education increasingly relies on shared clinical datasets. Safeguards must be established to ensure secure data handling and compliance with privacy regulations[56]. Finally, AI integration must avoid diminishing essential humanistic aspects of medicine, such as doctor-patient communication and mentorship in medical education. Ethical frameworks that emphasize explainability, fairness, and responsible use are therefore critical to maintaining professional integrity and patient trust[54,57].
Global health equity implications
AI-enabled education and clinical tools hold the potential to narrow gaps in access to quality training and care, especially in resource-limited and underserved regions[58]. Low-cost, AI-driven simulation platforms and online adaptive curricula can democratize access to advanced trauma orthopedic training, reducing dependence on high-cost cadaver labs or overseas fellowships. Similarly, AI-powered diagnostic support can augment the capacity of junior surgeons or practitioners in remote areas, ensuring timely and accurate decision making where senior expertise is scarce[58]. However, the benefits of AI may also inadvertently exacerbate inequities if deployment remains restricted to high-income settings with advanced infrastructure. Barriers such as digital divides, limited internet access, and high implementation costs could further disadvantage low-resource communities[56]. To achieve global health equity, international collaborations, open-access AI platforms, and policy initiatives are required to ensure affordable, scalable, and context-appropriate AI solutions that genuinely support universal access to trauma care education and services.
LIMITATIONS OF AI IN ORTHOPEDIC TRAUMA
Recent advances highlight the considerable potential of AI in orthopaedic trauma for imaging diagnostics, surgical planning, and postoperative outcome prediction. These developments promise improvements in diagnostic precision, preoperative decision making, and individualized treatment strategies. However, multiple fundamental limitations continue to impede clinical translation.
Data quality and representativeness remain primary barriers. Imaging datasets in trauma research frequently originate from single-center cohorts with limited sample sizes and heterogeneous acquisition protocols. Such constraints increase the risk of overfitting and reduce model generalizability across broader patient populations. Dijkstra et al. conducted a systematic review following the Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD) statement and the Prediction model Risk Of Bias ASsessment Tool (PROBAST) criteria and identified pervasive deficiencies in external validation and transparent reporting, with a high risk of bias[59]. Tian et al. emphasized the same challenges, noting persistent heterogeneity in imaging quality, inadequate sample sizes, and a lack of standardization[35]. Debs et al. similarly underscored that data variability and the absence of harmonized imaging protocols undermine the reproducibility and scalability of musculoskeletal AI models[60].
Methodological rigor and reporting transparency remain insufficient. Many orthopedic trauma AI studies omit robust external validation, a critical step for establishing model performance on independent datasets. Adherence to reporting standards such as TRIPOD is limited, constraining reproducibility and cross-study comparability. Lisacek-Kiosoglous highlighted the persistent influence of selection bias and questioned the clinical reliability of AI findings[52]. Debs and Fayad further identified incomplete disclosure of model architecture, training methods, and performance metrics as a persistent obstacle to clinical adoption[60].
The intrinsic opacity of deep learning models constitutes another major concern. Complex architectures often produce predictions without clear mechanistic explanations. Alzubaidi et al. reported that differences in image quality and clinical heterogeneity exacerbate interpretability challenges and compromise model robustness[61]. Tafat et al. noted that the absence of clinically meaningful explainability continues to undermine surgeon confidence[62].
Demographic variation and technical heterogeneity introduce additional sources of bias. Age, sex, ethnicity, comorbidities, scanner types, and acquisition protocols can produce systematic errors and inequitable outcomes. Koçak et al. detailed the origins, detection, and mitigation of such bias, underscoring its relevance to trauma imaging. These disparities reduce predictive accuracy and threaten the equitable application of AI across diverse clinical settings[63].
The integration of AI into routine workflows faces persistent regulatory and ethical obstacles. Data privacy protection, algorithmic accountability, and uncertainty in legal liability for diagnostic errors remain unresolved. Standardized frameworks for safety verification are lacking. Winkler et al. provided a practical guide outlining risk management and regulatory compliance requirements for medical AI implementation[64]. Further technical, ethical, and regulatory barriers have been identified that continue to delay clinical deployment[62].
Future work must prioritize multicenter high-quality data collection with harmonized imaging protocols and well-curated metadata. Enhanced model interpretability is needed, which can be achieved through the development and rigorous validation of explainable AI methods that deliver clinically actionable insights. Bias detection and mitigation strategies should be embedded in model development and evaluation. Internationally accepted regulatory and safety standards must guide approval, monitoring, and post-deployment surveillance. Coordinated efforts among clinicians, data scientists, and regulatory agencies will be essential for the safe, ethical, and sustainable integration of AI in orthopedic trauma.
LIMITATIONS OF THIS REVIEW
This review has several limitations. First, the literature search was limited to English-language publications, which may have excluded relevant studies published in other languages. Second, studies from low- and middle-income countries remain underrepresented, which may limit the global generalizability of our findings. Third, some of the evidence cited is derived from cross-sectional surveys or expert opinions, which provide limited evidence strength. Finally, due to the rapidly evolving nature of AI research, some emerging studies may not have been captured in this review despite our efforts to include the most recent evidence.
PRACTICAL IMPLICATIONS FOR IMPLEMENTATION
The findings of this review provide several practical implications for the integration of AI into continuing education in trauma orthopedics. First, hospitals should prioritize AI adoption in areas with the strongest supporting evidence, such as imaging diagnostics and VR-based surgical simulation. Second, implementation strategies should be tiered: tertiary hospitals can serve as pilot centers, while regional and community hospitals gradually adopt AI tools in accordance with infrastructure readiness. Third, structured AI training programs for educators are essential to ensure faculty competence in both technical and ethical aspects of AI use. Lastly, collaboration with policymakers is necessary to establish regulatory frameworks that promote safe, equitable, and sustainable AI adoption.
CONCLUSION
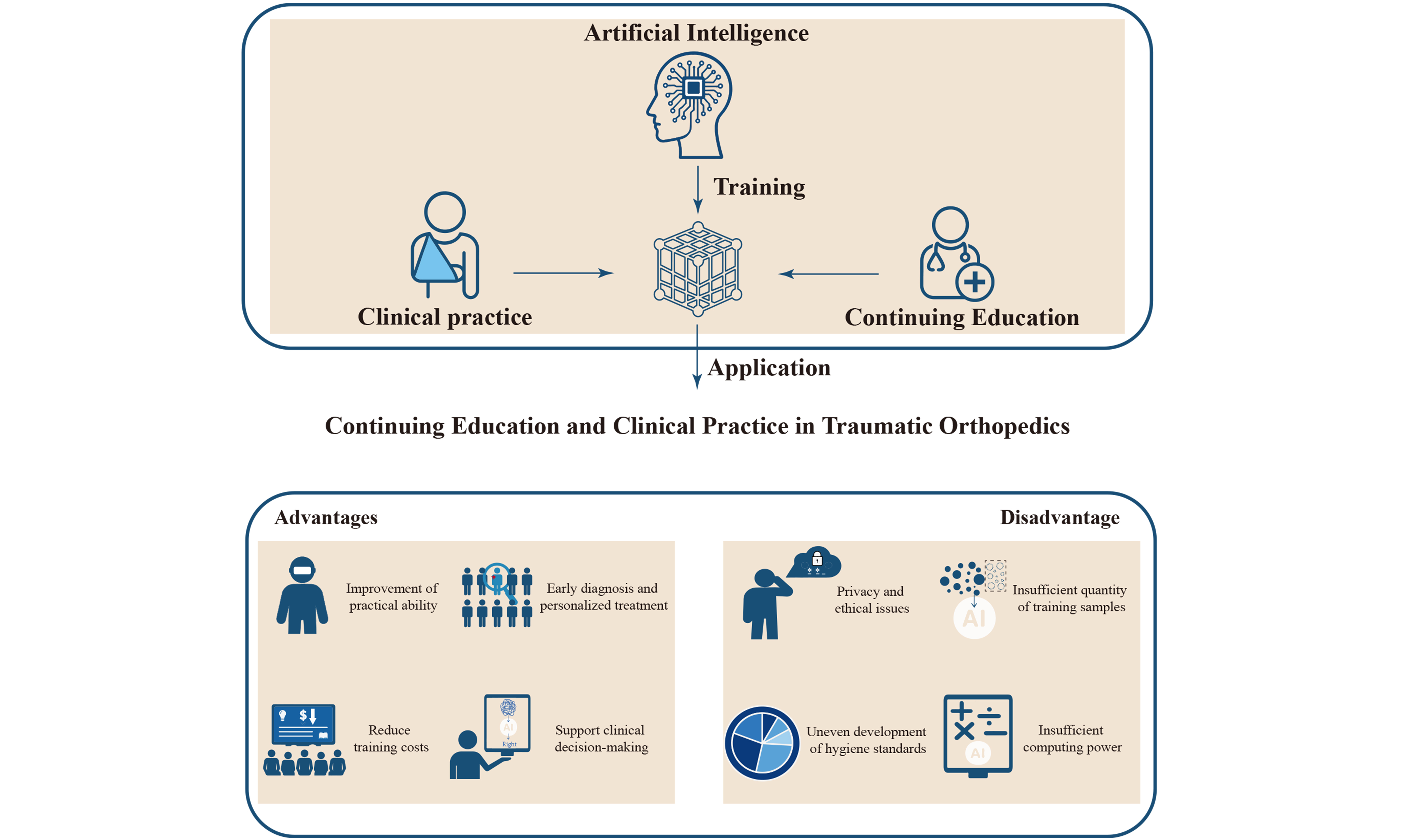
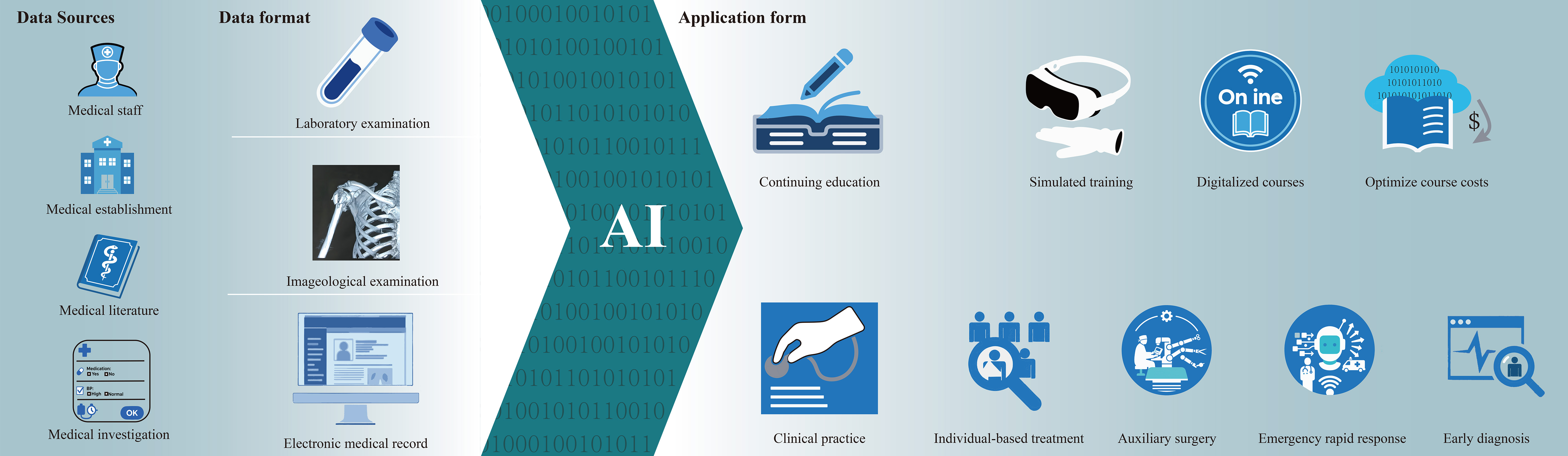
The integration of AI and advanced technologies in trauma orthopedics has transformed continuing medical education and clinical practice [Figure 1], with simulation training, cost-effective curricula, and digital tools significantly enhancing surgical skill acquisition, clinical decision making, and personalized learning. AI-driven systems demonstrate exceptional potential in imaging diagnostics, surgical navigation, and outcome prediction, while VR/AR platforms provide immersive training environments. Nevertheless, challenges remain, including data scarcity, model interpretability, ethical concerns, and inequitable global adoption. Additionally, the limitations of this review - such as potential language bias due to exclusion of non-English studies and the underrepresentation of research from low-resource regions - may affect the generalizability of the findings. Future advancements should prioritize standardized evaluation frameworks, longitudinal competency validation, and ethical guidelines to ensure the safe and equitable integration of AI. Collaborative efforts among educators, clinicians, and technologists will be essential to drive sustainable innovation, ultimately improving patient outcomes and ushering in a new era of intelligent orthopedic care.
Figure 1. The pivotal role of artificial intelligence (AI) in transforming continuing medical education and clinical practice in trauma orthopedics. The diagram shows that AI systems collect data from multiple sources - including healthcare professionals, medical institutions, scientific literature, and medical surveys. These data encompass laboratory tests, imaging examinations, and electronic medical records. AI integrates and analyzes these data intelligently, producing processed information that is ultimately applied to continuing education and clinical practice. Specifically, in continuing education, AI plays a significant role in simulation-based training, curriculum cost optimization, and digital learning. In clinical practice, its impact is particularly prominent in four areas: personalized treatment, surgical assistance, rapid response in emergency care, and early diagnosis. AI: Artificial intelligence; BP: blood pressure.
DECLARATIONS
Authors’ contributions
Made substantial contributions to the conception and design of the study and performed data analysis and interpretation: Zhu K, An Z, Zhang Y, Zhang Q
Performed data acquisition and provided administrative, technical, and material support: Liu J, Mao Y, Zhao R
Availability of data and materials
Not applicable.
Financial support and sponsorship
This study was supported by the Natural Science Research Project of Anhui Educational Committee (2024AH051233), the Science Research Project of Anhui Health Commission (AHWJ2023A30070), the Medical Innovation Foundation from Spinal Deformity Clinical Medicine and Research Center of Anhui Province (AHJZJX-GG2023-004), the Health Research Project of Bengbu City (BBWK2024C205), the Natural Science Research Project of Bengbu Medical University (2024byzd129), the Excellent Scientific Research and Innovation Team in Colleges and Universities of Anhui Province(2024AH010020), the Graduate Student Scientific Research Innovation Program (Byycx24089), and the Bengbu City Youth Project (BB25C060).
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2025.
REFERENCES
1. Stirling ER, Lewis TL, Ferran NA. Surgical skills simulation in trauma and orthopaedic training. J Orthop Surg Res. 2014;9:126.
2. Mackenzie CF, Tisherman SA, Shackelford S, Sevdalis N, Elster E, Bowyer MW. Efficacy of trauma surgery technical skills training courses. J Surg Educ. 2019;76:832-43.
3. Sadagopan NS, Prasad D, Jain R, Ahuja C, Dahdaleh NS, El Tecle NE. Beyond AI and robotics: the dawn of surgical automation in spine surgery. Art Int Surg. 2024;4:387-400.
4. Moran ME, George R. Past present and future of simulation in trauma. In: StatPearls [Internet]. Treasure Island: StatPearls Publishing; 2025.
5. Davies J, Pilling R, Dimri R, Chakrabarty G. Expert practical operative skills teaching in Trauma and Orthopaedics at a nominal cost. Surgeon. 2012;10:330-3.
6. Suárez ADP, Cepeda MP. Factores que intervienen en el aprendizaje de ortopedia y traumatología en estudiantes de instrumentación quirúrgica en una institución de educación superior en la ciudad de Bogotá. Educación Médica. 2021;22:323-9. (in Spanish).
7. Mehta S, Smith JM. Resources for your career in orthopaedic traumatology: what can the OTA do for you? J Orthop Trauma. 2012;26 Suppl 1:S25-6.
8. Maffulli N, Rodriguez HC, Stone IW, et al. Artificial intelligence and machine learning in orthopedic surgery: a systematic review protocol. J Orthop Surg Res. 2020;15:478.
9. Fuleihan AA, Menta AK, Azad TD, et al. Navigating artificial intelligence in spine surgery: implementation and optimization across the care continuum. Art Int Surg. 2024;4:288-95.
10. Cobianchi L, Piccolo D, Dal Mas F, et al; Team Dynamics Study Group. Correction: Surgeons’ perspectives on artificial intelligence to support clinical decision-making in trauma and emergency contexts: results from an international survey. World J Emerg Surg. 2023;18:22.
11. De Simone B, Abu-Zidan FM, Gumbs AA, et al. Knowledge, attitude, and practice of artificial intelligence in emergency and trauma surgery, the ARIES project: an international web-based survey. World J Emerg Surg. 2022;17:10.
12. Shah RM, Wong C, Arpey NC, Patel AA, Divi SN. A surgeon’s guide to understanding artificial intelligence and machine learning studies in orthopaedic surgery. Curr Rev Musculoskelet Med. 2022;15:121-32.
13. Checcucci E, De Cillis S, Amparore D, et al. Artificial intelligence alert systems during robotic surgery: a new potential tool to improve the safety of the intervention. Urol Video J. 2023;18:100221.
14. Zhu Z, Zheng G, Zhang C. Development and clinical application of robot-assisted technology in traumatic orthopedics. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36:915-22. (in Chinese).
15. Salimi M, Parry JA, Shahrokhi R, Mosalamiaghili S. Application of artificial intelligence in trauma orthopedics: limitation and prospects. World J Clin Cases. 2023;11:4231-40.
16. Powling AS, Lisacek-Kiosoglous AB, Fontalis A, Mazomenos E, Haddad FS. Unveiling the potential of artificial intelligence in orthopaedic surgery. Br J Hosp Med. 2023;84:1-5.
17. Jeyaraman M, Ratna HVK, Jeyaraman N, Venkatesan A, Ramasubramanian S, Yadav S. Leveraging artificial intelligence and machine learning in regenerative orthopedics: a paradigm shift in patient Care. Cureus. 2023;15:e49756.
18. Civaner MM, Uncu Y, Bulut F, Chalil EG, Tatli A. Artificial intelligence in medical education: a cross-sectional needs assessment. BMC Med Educ. 2022;22:772.
19. Ejaz H, McGrath H, Wong BL, Guise A, Vercauteren T, Shapey J. Artificial intelligence and medical education: a global mixed-methods study of medical students’ perspectives. Digit Health. 2022;8:20552076221089099.
20. Boillat T, Nawaz FA, Rivas H. Readiness to embrace artificial intelligence among medical doctors and students: questionnaire-based study. JMIR Med Educ. 2022;8:e34973.
21. Bhattad PB, Jain V. Artificial intelligence in modern medicine - the evolving necessity of the present and role in transforming the future of medical care. Cureus. 2020;12:e8041.
22. Busch F, Adams LC, Bressem KK. Biomedical ethical aspects towards the implementation of artificial intelligence in medical education. Med Sci Educ. 2023;33:1007-12.
23. Krive J, Isola M, Chang L, Patel T, Anderson M, Sreedhar R. Grounded in reality: artificial intelligence in medical education. JAMIA Open. 2023;6:ooad037.
25. Narayanan S, Ramakrishnan R, Durairaj E, Das A. Artificial intelligence revolutionizing the field of medical education. Cureus. 2023;15:e49604.
26. Boddu S, Subramanian A, Sattar ZS, et al. Utility of artificial intelligence-based tool for medical education during rounds in the ICU. CHEST. 2023;164:A1809.
27. Beam AL, Drazen JM, Kohane IS, Leong TY, Manrai AK, Rubin EJ. Artificial intelligence in medicine. N Engl J Med. 2023;388:1220-1.
28. Wartman SA, Combs CD. Reimagining medical education in the age of AI. AMA J Ethics. 2019;21:E146-152.
29. Aggarwal R, Mytton OT, Derbrew M, et al. Training and simulation for patient safety. Qual Saf Health Care. 2010;19 Suppl 2:i34-43.
30. Loftus TJ, Filiberto AC, Balch J, et al. Intelligent, autonomous machines in surgery. J Surg Res. 2020;253:92-9.
31. Vitiello V, Lee SL, Cundy TP, Yang GZ. Emerging robotic platforms for minimally invasive surgery. IEEE Rev Biomed Eng. 2013;6:111-26.
32. Bilgic E, Gorgy A, Yang A, et al. Exploring the roles of artificial intelligence in surgical education: a scoping review. Am J Surg. 2022;224:205-16.
33. Misir A. Artificial intelligence in orthopedic trauma: a comprehensive review. Injury. 2025;56:112570.
34. Milella F, Famiglini L, Banfi G, Cabitza F. Application of machine learning to improve appropriateness of treatment in an orthopaedic setting of personalized medicine. J Pers Med. 2022;12:1706.
35. Tian C, Gao Y, Rui C, Qin S, Shi L, Rui Y. Artificial intelligence in orthopaedic trauma. EngMedicine. 2024;1:100020.
36. Mienye ID, Obaido G, Jere N, et al. A survey of explainable artificial intelligence in healthcare: concepts, applications, and challenges. Inform Med Unlocked. 2024;51:101587.
37. Hildt E. What is the role of explainability in medical artificial intelligence? Bioengineering. 2025;12:375.
38. Joseph J. Algorithmic bias in public health AI: a silent threat to equity in low-resource settings. Front Public Health. 2025;13:1643180.
39. Hussain SA, Bresnahan M, Zhuang J. Can artificial intelligence revolutionize healthcare in the Global South? Digit Health. 2025;11:20552076251348024.
40. Al-Saadawi A, Tehranchi S, Ahmed S, Nzeako OJ. Exploring the current applications of artificial intelligence in orthopaedic surgical training: a systematic scoping review. Cureus. 2025;17:e81671.
41. Appel G, Shahzad AT, Reopelle K, DiDonato S, Rusnack F, Papanagnou D. Exploring medical student experiences of trauma in the emergency department: opportunities for trauma-informed medical education. West J Emerg Med. 2024;25:828-37.
42. Tian C, Chen X, Zhu H, Qin S, Shi L, Rui Y. Application and prospect of machine learning in orthopaedic trauma. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2023;37:1562-8. (in Chinese).
43. Cabitza F, Locoro A, Banfi G. Machine learning in orthopedics: a literature review. Front Bioeng Biotechnol. 2018;6:75.
44. Spitler CA. Life long learning: the attending and educator in orthopedic trauma. Orthop Clin North Am. 2021;52:53-9.
45. Mackenzie CF, Garofalo E, Shackelford S, et al. Using an individual procedure score before and after the advanced surgical skills exposure for trauma course training to benchmark a hemorrhage-control performance metric. J Surg Educ. 2015;72:1278-89.
46. Kalraiya A, Buddhdev P. The TROJAN project: creating a customized international orthopedic training program for junior doctors. Orthop Rev. 2015;7:5750.
47. Hopkins L, Robinson DBT, Brown C, et al. Trauma and orthopedic surgery curriculum concordance: an operative learning curve trajectory perspective. J Surg Educ. 2019;76:1569-78.
48. Cannada LK. Orthopaedic trauma education: how many to train and how to pay for it? J Orthop Trauma. 2014;28 Suppl 10:S23-6.
49. Taylor BC, Fowler TT. Analysis of the trauma section of the orthopaedic in-training examination. Orthopedics. 2011;34:e261-6.
50. Haider Z, Hunter A. Orthopedic trainees’ perceptions of the educational value of daily trauma meetings. J Surg Educ. 2020;77:991-8.
51. Lisacek-Kiosoglous AB, Powling AS, Fontalis A, Gabr A, Mazomenos E, Haddad FS. Artificial intelligence in orthopaedic surgery. Bone Joint Res. 2023;12:447-54.
52. Knopp MI, Warm EJ, Weber D, et al. AI-enabled medical education: threads of change, promising futures, and risky realities across four potential future worlds. JMIR Med Educ. 2023;9:e50373.
53. Mennella C, Maniscalco U, De Pietro G, Esposito M. Ethical and regulatory challenges of AI technologies in healthcare: a narrative review. Heliyon. 2024;10:e26297.
54. Pressman SM, Borna S, Gomez-Cabello CA, Haider SA, Haider C, Forte AJ. AI and ethics: a systematic review of the ethical considerations of large language model use in surgery research. Healthcare. 2024;12:825.
55. Berdahl CT, Baker L, Mann S, Osoba O, Girosi F. Strategies to improve the impact of artificial intelligence on health equity: scoping review. JMIR AI. 2023;2:e42936.
56. Badr J, Motulsky A, Denis JL. Digital health technologies and inequalities: a scoping review of potential impacts and policy recommendations. Health Policy. 2024;146:105122.
57. Dychiao RG, Nazer L, Mlombwa D, Celi LA. Artificial intelligence and global health equity. BMJ. 2024;387:q2194.
58. Zuhair V, Babar A, Ali R, et al. Exploring the impact of artificial intelligence on global health and enhancing healthcare in developing nations. J Prim Care Community Health. 2024;15:21501319241245847.
59. Dijkstra H, van de Kuit A, de Groot TM, et al; Machine Learning Consortium. Systematic review of machine-learning models in orthopaedic trauma. Bone Jt Open. 2024;5:9-19.
60. Debs P, Fayad LM. The promise and limitations of artificial intelligence in musculoskeletal imaging. Front Radiol. 2023;3:1242902.
61. Alzubaidi L, Al-Dulaimi K, Salhi A, et al. Comprehensive review of deep learning in orthopaedics: applications, challenges, trustworthiness, and fusion. Artif Intell Med. 2024;155:102935.
62. Tafat W, Budka M, Mcdonald D, Wainwright TW. Artificial intelligence in orthopaedic surgery: A comprehensive review of current innovations and future directions. Comput Struct Biotechnol Rep. 2024;1:100006.
63. Koçak B, Ponsiglione A, Stanzione A, et al. Bias in artificial intelligence for medical imaging: fundamentals, detection, avoidance, mitigation, challenges, ethics, and prospects. Diagn Interv Radiol. 2025;31:75-88.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Copyright
Data & Comments
Data

















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at [email protected].