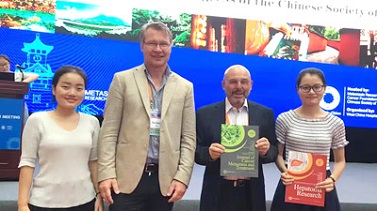
Special Interview with Prof. Gregory J. Gores, Medicine and Physiology, Mayo Clinic
On August 6, 2025, the Editorial Office of Hepatoma Research conducted an interview with Prof. Gregory J. Gores, Professor of Medicine and Physiology at Mayo Clinic, Rochester, USA. Prof. Gores discussed the role of CD4⁺ T cells in driving fibrosis in metabolic dysfunction-associated steatohepatitis (MASH), compared liver resection and transplantation in perihilar cholangiocarcinoma (pCCA), summarized key points from the Milan Jury-Based Consensus, and outlined the application of AI and high-throughput technologies in hepatobiliary tumor management. He concluded by advising young scientists to use AI appropriately—not as a replacement for expertise, but as a tool to advance medical progress.
Introduction to the Interviewee

Prof. Gregory J. Gores, M.D., is Professor of Medicine and Physiology at Mayo Clinic, Rochester, Minnesota, USA, and serves as Executive Dean for Research for the Mayo Clinic enterprise. He is also a consultant in the Division of Gastroenterology and Hepatology, Department of Internal Medicine.
His research focuses on the molecular mechanisms of liver cell injury, including apoptosis in cholestatic and fatty liver diseases, as well as mechanisms by which cancer cells evade programmed cell death. He has led translational and clinical studies in hepatobiliary cancers, including hepatocellular carcinoma and cholangiocarcinoma.
Prof. Gores is a past president of the American Association for the Study of Liver Diseases (AASLD) and the International Liver Cancer Association (ILCA), and has held leadership roles in the American Gastroenterological Association and the American Society of Transplant Surgeons. He currently serves as Editor-in-Chief of Hepatology (2022–2026).
Questions
Q1: In your team’s recent study, CD4⁺ T cells were shown to promote fibrosis in metabolic dysfunction-associated steatohepatitis (MASH). Could you explain the specific mechanisms by which CD4⁺ T cells contribute to fibrosis development in MASH, and how they interact with other immune cells?
Q2: Your recent study compared liver resection—with or without vascular resection—and liver transplantation in patients with perihilar cholangiocarcinoma (pCCA). What are the main advantages and challenges of liver resection versus liver transplantation for treating pCCA patients?
Q3: You contributed to the development of the Recommendations on Perihilar Cholangiocarcinoma: The Milan Jury-Based Consensus. Could you highlight the key diagnostic and therapeutic recommendations from this consensus?
Q4: With the continuous advancement of artificial intelligence and high-throughput technologies, how is your team leveraging these tools to improve the early diagnosis and treatment of hepatobiliary tumors?
Q5: As an experienced researcher, what advice would you give to young scientists interested in pursuing basic and clinical research in hepatobiliary cancers?
Stay tuned to Hepatoma Research for more exclusive interviews with global leaders advancing liver cancer research and precision oncology.
Managing Editor: Victoria Lee
Language Editor: Catherine Yang
Production Editor: Ting Xu
Respectfully Submitted by the Editorial Office of Hepatoma Research