Innovation in aortic surgery requires more than AI: a perspective on data governance and shared decision-making
Abstract
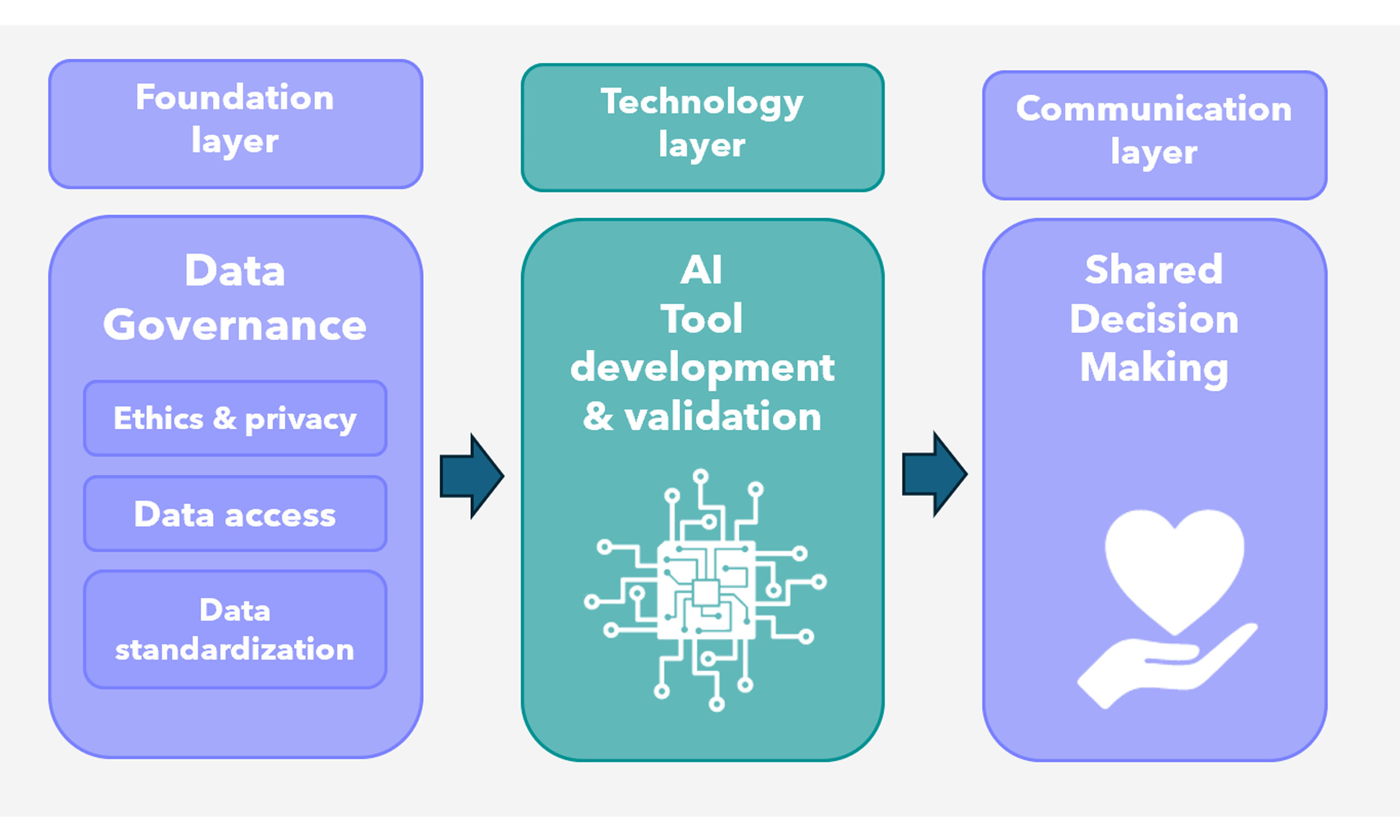
Clinical decision-making for individuals undergoing valvular and aortic surgery remains challenging, particularly in young patients facing lifelong risk and repeated interventions. As predictive technologies such as artificial intelligence and advanced statistical modelling evolve, the surgical community must ensure that key foundational elements, namely data governance, including data standardization, and regulation, are firmly in place. Without high-quality, standardized, and ethically governed data, predictive models risk offering misleading guidance rather than meaningful personalization. While data governance ensures the scientific robustness of predictive technologies, shared decision-making (SDM) ensures these innovations remain closely aligned with the lived experiences, values, and preferences of individual patients. This perspective emphasizes that advancing decision-making in aortic surgery requires deliberate investment in building data ecosystems and fostering SDM communication practices, ensuring that innovation is both scientifically sound and truly responsive to patient needs.
Keywords
INTRODUCTION
Selecting the optimal treatment for patients with aortic and valvular disease requires integrating scientific evidence from trials and large databases with the unique clinical profile and informed preferences of each patient. Historically, many therapeutic decisions were based on a “one-size-fits-all” approach, largely due to challenges in appropriate patient risk stratification, timing of surgery, anatomical variability, surgical treatment options, and capturing informed patient preferences.
This complexity becomes especially apparent in certain clinically relevant scenarios. For example, when managing a patient with mild aortic root dilation and severe aortic regurgitation, should the aortic root be replaced despite no clear surgical indication? Or how should we respond to a patient with a 45-millimeter ascending aortic aneurysm who insists on surgery to eliminate the “ticking time bomb” anxiety?
This paper aims to identify the key challenges for the surgical community in generating evidence based on big data and integrating it with individual patient needs and preferences, highlighting focus points for further efforts in the personalization (research) of the management of aortic and valvular disease.
TECHNICAL INNOVATION: FOCUS ON DATA GOVERNANCE
Recent literature has highlighted the potential of advanced statistical models, machine learning, and artificial intelligence (AI) to advance patient-specific treatment planning[1]. In 2022 alone, the Food and Drug Administration approved more than 100 AI algorithms/devices[2]. However, for these AI-based solutions to succeed, they must be supported by foundational elements provided by clinicians with domain knowledge and insight into the surgical community. Commonly captured under the umbrella term “Data Governance”, this concept encompasses the system of decision rights and accountabilities for information-related processes, implemented according to agreed-upon models that specify who can take which actions with what information, when, under what circumstances, and using what methods[3]. Several subcategories of data governance may need specific attention from the aortic surgical community: Data Ethics and Privacy, Data Standardization, and Data Access and Policies.
(Big) Data ethics and privacy
Apart from conventional risk factors such as age, sex and comorbidities, current evidence is increasingly pointing towards novel risk factors, such as aortic length, tissue characteristics that can help optimize patient-tailored disease management[4]. In the context of big data research, researchers often do not know in advance which risk factors will prove relevant, requiring the collection of a wide range of potential variables, potentially by linking different datasets. However, traditional informed consent models, originally designed for clinical research, are not well-suited to the demands of big data studies[5]. Ethical and legal communities are actively reexamining consent and privacy frameworks[6]. A pressing practical challenge is the lack of consensus among ethical review boards, with differing interpretations of ethical data collection threatening the cross-institutional collaboration crucial for building robust big data repositories. Therefore, it is essential for the surgical community to engage proactively in these discussions, ensuring that research feasibility, collaboration, and the promotion of public good are appropriately balanced against the potential risks associated with large-scale data collection.
Data standardization
Beyond harmonizing ethical and legal standards, the standardization of the data itself is a critical prerequisite for the success of big data research initiatives. Variability in how data are collected, labeled, measured, and stored across different centers can severely limit the interoperability and comparability of datasets. Establishing consensus on core data elements, uniform measurement protocols, and shared ontologies is therefore essential not only for facilitating collaboration but also for ensuring scientific reproducibility, data quality, and patient safety. Domain experts (clinicians) should be deeply involved in these standardization efforts. A recently developed standard set for aortic and heart valve disease by the International Consortium for Health Outcomes Measurement (ICHOM) spearheads these efforts, and was achieved by a close collaboration of researchers, clinicians and patients[7]. Similarly, the Observational Medical Outcomes Partnership (OMOP) Common Data Model (CDM) provides a standardized framework for structuring observational data, enabling its effective use in AI and machine learning applications to better predict patient outcomes[8].
Data access and policies
Broad collaborations including national and international databases have already significantly contributed to research regarding aortic and valvular surgery and provided some patient-specific outcomes that can be used for patient-tailoring. Examples include the Heart Valve Society Aortic Valve database and the European Association of Cardiothoracic Surgery Adult Cardiac Database[9,10]. Transparent access mechanisms in these databases, with opt-out options for data suppliers, enhance trust and enable impactful big data research. For example, findings from these large datasets have altered clinical practice: there was previously reluctance to repair bicuspid aortic valves due to concerns about repair durability. However, newer evidence demonstrates that bicuspid aortic valve repair can yield outcomes comparable to tricuspid aortic valve repair, resulting in greater acceptance and expanded surgical indications[11].
With these foundational elements firmly established, true advances in AI and machine learning to predict individualized outcomes are in the immediate future.
SOCIAL INNOVATION: FOCUS ON IMPLEMENTING SHARED DECISION-MAKING IN CLINICAL PRACTICE
While technological advances offer powerful tools, their full potential will only be realized through a complementary social innovation: shared decision-making (SDM).
Eric Topol, in his book Deep Medicine, envisions a transformative future where clinicians spend less time on administrative tasks and more time in meaningful patient dialogue[12]. Achieving this vision, however, demands a fundamental shift in clinician and patient behavior. Communication must be prioritized alongside data-driven clinical reasoning.
Predictive modeling and AI-driven tools can enhance personalized risk assessments, such as modeling the likelihood of aortic rupture, but they cannot replace discussions of a patient’s unique values and fears. A predictive model may recommend watchful waiting for a 45 mm aortic root aneurysm; yet, if a patient experiences significant anxiety, early surgery might better align with their personal goals. Few practical examples of advanced technologies such as AI and digital twins exist in current practice for patients with aortic disease. A recent case study demonstrated it is possible to use digital twins to help plan aortic replacement procedures[13]. Another example is the use of deep learning algorithms to automatically measure the aortic geometry, to achieve standardized and reproducible measurements[14].
Structured frameworks, such as patient portals, decision aids, and Patient-Reported Outcome Measures (PROMs)/Patient-Reported Experience Measures (PREMs), are essential for embedding SDM in daily practice. Decision aids, in particular, have been shown to help both patients and clinicians engage more effectively[15].
A practical model by Stiggelbout et al. outlines four key steps for SDM[16]:
1. Inform the patient that a decision needs to be made and that their input is crucial.
2. Explain the available options, including benefits and risks.
3. Elicit and discuss the patient's values and preferences.
4. Make or defer the decision based on the patient's informed preferences.
Successful implementation demands dedicated education, training, and resource allocation, fostering communication competencies crucial for truly personalized aortic management.
CONCLUSION
Driving innovation in aortic surgery requires a wider focus than technological algorithms alone; it also requires a dual investment in data ecosystems and human-centered communication. By prioritizing clinician engagement in data governance and training in SDM, we can ensure that future advances are both scientifically robust and truly responsive to individual patient needs and values.
DECLARATIONS
Acknowledgment
The Graphical Abstract was created using BioRender.
Author contributions
Drafted the perspective and prepared the visualizations: de Keijzer AR, Rhellab R, Zito F
Provided supervision and reviewed the manuscript: Kluin J, Melina G, Takkenberg JJM, Veen KM
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2026.
REFERENCES
1. Vaidya YP, Shumway SJ. Artificial intelligence: the future of cardiothoracic surgery. J Thorac Cardiovasc Surg. 2025;169:1265-70.
2. Joshi G, Jain A, Araveeti SR, Adhikari S, Garg H, Bhandari M. FDA-approved artificial intelligence and machine learning (AI/ML)-enabled medical devices: an updated landscape. Electronics. 2024;13:498.
3. The Data Governance Basics. Definitions of data governance. Available from https://datagovernance.com/the-data-governance-basics/definitions-of-data-governance/ [accessed 09 February 2026].
4. Thijssen CGE, Dekker S, Bons LR, et al. Novel biomarkers associated with thoracic aortic disease. Int J Cardiol. 2023;378:115-22.
5. McKeown A, Mourby M, Harrison P, Walker S, Sheehan M, Singh I. Ethical issues in consent for the reuse of data in health data platforms. Sci Eng Ethics. 2021;27:9.
6. Ienca M, Ferretti A, Hurst S, Puhan M, Lovis C, Vayena E. Considerations for ethics review of big data health research: a scoping review. PLoS One. 2018;13:e0204937.
7. Lansac E, Veen KM, Joseph A, et al. The first international consortium for health outcomes measurement (ICHOM) standard dataset for reporting outcomes in heart valve disease: moving from device- to patient-centered outcomes. Circ Cardiovasc Qual Outcomes. 2025;18:e000128.
8. Ohdsi. The Book of OHDSI: Observational Health Data Sciences and Informatics. OHDSI, 2019. Available from https://www.amazon.com/OHDSI-Observational-Health-Sciences-Informatics/dp/1088855199 [accessed 09 February 2026].
9. van der Ven CC, Kluin J, Takkenberg JJ, et al.; on behalf of the Aortic Valve Research Network Investigators. Data Resource Profile: Heart Valve Society Aortic Valve Database (HVS AV Database). J Heart Valve Soc. 2024;1:30494826241296370.
10. EACTS. EACTS Adult Cardiac Database. Available from https://www.eacts.org/quality-improvement/adult-cardiac-database/ [accessed 09 February 2026].
11. Jasinski MJ, Kosiorowska K, Gocol R, et al. Bicuspid aortic valve repair: outcomes after 17 years of experience. Eur J Cardiothorac Surg. 2021;60:1053-61.
12. Topol E. Deep medicine: how artificial intelligence can make healthcare human again. 1th ed. Basic Books, 2019. Available from https://www.amazon.com/Deep-Medicine-Artificial-Intelligence-Healthcare/dp/1541644638 [accessed 09 February 2026].
13. Creazzo G, Nannini G, Saitta S, et al. Deployment of a digital twin using the coupled momentum method for fluid-structure interaction: a case study for aortic aneurysm. Comput Biol Med. 2025;190:110084.
14. Bratt A, Blezek DJ, Ryan WJ, et al. Deep learning improves the temporal reproducibility of aortic measurement. J Digit Imaging. 2021;34:1183-9.
15. Korteland NM, Ahmed Y, Koolbergen DR, et al. Does the use of a decision aid improve decision making in prosthetic heart valve selection? A multicenter randomized trial. Circ Cardiovasc Qual Outcomes. 2017;10:e003178.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Special Topic
Copyright
Data & Comments
Data
















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at [email protected].