Predictors of short-term mortality in patients undergoing emergency coronary artery bypass grafting: a systematic review and meta-analysis
Abstract
Aim: Emergency coronary artery bypass grafting (CABG) is a critical intervention for patients with acute coronary syndrome (ACS), particularly in high-risk cases where rapid revascularization is necessary. Despite advancements in surgical techniques, early mortality rates remain high. This study aims to identify predictors of short-term mortality in patients undergoing emergency CABG for ACS through a comprehensive systematic review and meta-analysis.
Methods: A PRISMA-based systematic review was performed using major databases up to May 2024. Inclusion criteria focused on studies reporting short-term mortality outcomes and associated predictors in patients undergoing emergency CABG for ACS. Data extraction and quality assessment were performed independently by multiple reviewers. Statistical analysis included pooled odds ratios (OR) and confidence intervals (CI) for identified predictors using random-effects models.
Results: A total of 20 studies encompassing 4,777 patients met the inclusion criteria. Key predictors of short-term mortality include advanced age (OR 1.40, 95%CI: 1.07-1.82), cardiogenic shock (OR 5.35, 95%CI: 3.27-8.74), chronic kidney disease (OR 3.55, 95%CI: 1.30-9.71), and preoperative use of an intra-aortic balloon pump (OR 2.46, 95%CI: 1.00-6.04). Timing of surgery within the first 48 h post-ACS was also associated with higher mortality rates.
Conclusion: This systematic review and meta-analysis highlight important predictors of short-term mortality in patients undergoing emergency CABG for ACS. These findings underscore the importance of tailored perioperative management strategies to improve outcomes in this high-risk patient population.
Keywords
INTRODUCTION
Acute coronary syndrome (ACS) represents a spectrum of urgent cardiac conditions that require immediate and specialized management[1]. Treatment strategies for ACS are tailored to the specific presentation, with distinct protocols for ST-Elevation Myocardial Infarction (STEMI) and Non-ST-Elevation Myocardial Infarction (NSTEMI)[2]. For STEMI, rapid reperfusion via Primary Percutaneous Coronary Intervention (PCI) is the primary goal, with fibrinolytic therapy as an alternative when PCI is unavailable[3]. Alternatively, the guidelines for managing NSTEMI advise implementing an early invasive approach within 24 h for patients identified as high-risk, which includes those with elevated cardiac biomarkers, diabetes, high GRACE scores, or older age. This approach is designed to reduce recurrent ischemia and potentially decrease mortality[4].
The decision between PCI and coronary artery bypass grafting (CABG) for revascularization in ACS patients is influenced by various factors, such as the patient’s clinical condition, comorbidities, and the extent and complexity of coronary artery disease (CAD), which is frequently evaluated using the SYNTAX score[5]. CABG is essential for patients with complex coronary diseases, such as multivessel or left main disease[6]. While extensive research has compared PCI to CABG, there is a notable gap in studies specifically analyzing the outcomes and predictors of mortality for patients undergoing emergency CABG, particularly within the first 30 days post-surgery.
Emergency CABG is often performed in critical situations where immediate revascularization is necessary due to ongoing ischemia, angiographic complications, or the presence of complex multivessel disease unsuitable for PCI[7]. Despite improvements in surgical techniques and perioperative care, early mortality rates for emergency CABG remain high[8], emphasizing the need to identify predictors of short-term mortality to enhance patient outcomes and tailor perioperative management strategies effectively.
This systematic review and meta-analysis aim to address the current literature gap by identifying predictors of short-term mortality in patients undergoing emergency CABG for ACS. By consolidating existing data, this study strives to offer a thorough understanding of the risk factors linked to early mortality, providing valuable insights to guide clinical practice, enhance risk stratification, and optimize perioperative care.
METHODS
Search strategy
We performed a systematic literature review following the PRISMA guidelines[9]. Extensive searches were carried out in OVID MEDLINE®, EMBASE, SCOPUS, and PUBMED from the inception until May 2024. The search terms included (“Acute Coronary Syndrome”[Mesh] OR “ACS” OR “Acute Coronary Syndromes” OR “Non-ST-Elevation Myocardial Infarction”[Mesh] OR “NSTEMI” OR “Non-ST-Elevation Myocardial Infarctions”) AND (“Coronary Artery Bypass”[Mesh] OR “CABG” OR “Coronary Artery Bypass Grafting” OR “Coronary Artery Bypass Surgery”) AND (“Off-Pump Coronary Artery Bypass”[Mesh] OR “Off-Pump CABG” OR “OPCAB” OR “Off-Pump Coronary Artery Bypass Grafting” OR “On-Pump Coronary Artery Bypass”[Mesh] OR “On-Pump CABG” OR “ONCAB” OR “On-Pump Coronary Artery Bypass Grafting”).
Study selection
The studies located through the search strategy were assessed for inclusion according to predefined criteria. The criteria for inclusion were: 1) human subjects; 2) retrospective, prospective studies, or randomized control trials (RCTs); 3) reporting short-term (≤ 30 days) mortality in patients undergoing emergency CABG (< 72 h) for ACS; 4) studies employing univariate or multivariate regression analysis to analyze the identified risk factors; 5) results presented as odds ratio (OR) with 95% confidence interval (CI), or providing data necessary to calculate OR. Exclusion criteria included: 1) studies conducted on animals; 2) non-English studies; 3) studies reporting mid- or long-term mortality (> 30 days).
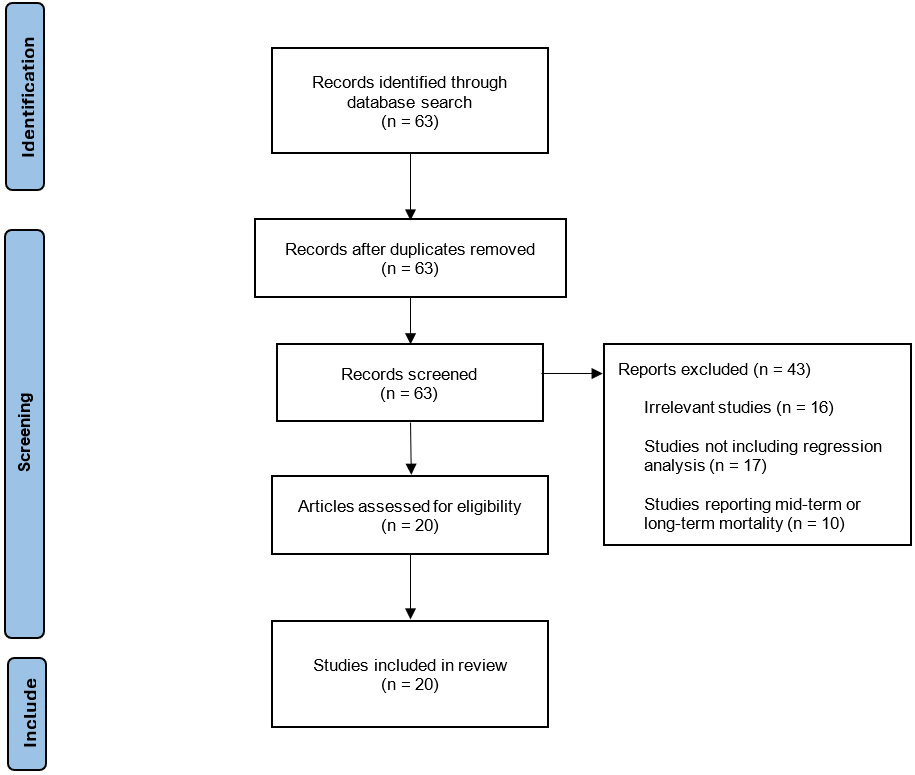
Two reviewers independently (MC, BN) screened the titles and abstracts of the identified studies, and then conducted a full-text review to verify eligibility. Any discrepancies were addressed through discussion or by consulting a third reviewer (SGR), ensuring an accurate and unbiased selection of studies. The study selection process followed strict PRISMA guidelines to ensure transparency and minimize selection bias. A detailed PRISMA flow diagram illustrating this process is shown in Figure 1.
Data extraction and quality assessment
Two independent reviewers extracted data, which encompassed details such as publication year, authorship, patient demographics, inclusion/exclusion criteria, cardiac risk factors, descriptions of interventions, and outcome definitions and events [Table 1]. The Revised Cochrane risk-of-bias 2 (RoB 2) tool was employed to assess bias in randomized studies[10]. For observational studies, the Risk of Bias In Non-randomized Studies of Interventions (ROBINS-I) scale was utilized[11].
Studies characteristics
| Study | Study design | Country | Study period | Type of ACS | Time to surgery | Number of patients |
| Locker et al., 2000[23] | Retrospective | Israel | 1992-1998 | NSTEMI, STEMI | ≤ 48 h | 77 |
| Hirose et al., 2002[24] | Retrospective | Japan | 1991-2001 | NSTEMI, STEMI | ≤ 48 h | 159 |
| Ochi et al., 2003[25] | Retrospective | Japan | 1998-2001 | UA, NSTEMI, STEMI | ≤ 24 h | 72 |
| Kerendi et al., 2005[26] | Retrospective | USA | 1996-2003 | NSTEMI, STEMI | ≤ 24 h | 614 |
| Onorati et al., 2005[27] | Prospective | Italy | 2002-2004 | UA, NSTEMI | NR | 262 |
| Thielmann et al., 2006[28] | Prospective | Germany | 2000-2005 | NSTEMI, STEMI | ≤ 24 h | 254 |
| Darwazah et al., 2009[29] | Retrospective | Israel | 1999-2005 | NR | ≤ 24 h | 79 |
| Kaya et al., 2010[30] | Prospective | Turkey | 2006-2008 | UA, NSTEMI, STEMI | ≤ 6 h | 198 |
| Joskowiak et al., 2010[31] | Retrospective | Germany | 2002-2008 | NSTEMI, STEMI | ≤ 48 h | 158 |
| Martinez et al., 2010[32] | Retrospective | Singapore | 2002-2007 | UA, NSTEMI, STEMI | ≤ 24 h | 136 |
| Fattouch et al., 2011[33] | Retrospective | Italy | 2002-2007 | STEMI | ≤ 72 h | 207 |
| Sezai et al., 2012[34] | Retrospective | Japan | 1996-2009 | NSTEMI, STEMI | ≤ 24 h | 105 |
| Khaladj et al., 2013[35] | Prospective | Germany | 2009-2010 | NSTEMI, STEMI | ≤ 6 h | 127 |
| Hata et al., 2014[36] | Retrospective | Japan | 1994-2004 | UA, NSTEMI, STEMI | ≤ 48 h | 104 |
| Gaudino et al., 2015[37] | Prospective | Italy, Belgium | 2000-2011 | NSTEMI, STEMI | ≤ 72 h | 67 |
| Davierwala et al., 2016[38] | Retrospective | Germany | 2000-2014 | NSTEMI, STEMI | NR | 508 |
| Grothusen et al., 2017[19] | Retrospective | Germany | 2001-2015 | NSTEMI, STEMI | ≤ 48 h | 766 |
| Hung et al., 2021[39] | Retrospective | Vietnam | 2017-2019 | NSTEMI, STEMI | ≤ 48 h | 71 |
| Bianchi et al., 2022[40] | Retrospective | Italy | 2009-2020 | NSTEMI, STEMI | NR | 430 |
| Tekin et al., 2023[41] | Retrospective | Turkey | 2010-2020 | NR | ≤ 12 h | 383 |
Data analysis
All analyses were executed using Review Manager (RevMan) Version 5.4.1, developed by The Nordic Cochrane Centre in Copenhagen, Denmark. The combined effect size was denoted by the OR and its 95%CI. To account for inter-study variability and ensure more cautious CIs given heterogeneity, random-effects models were applied[12]. Statistical heterogeneity across studies was evaluated using the I² statistic, which reflects the proportion of overall variability attributed to differences between studies rather than random variation. We adhered to standard guidelines for interpreting heterogeneity: low (I2 = 25% to 49%), moderate (I2 = 50% to 74%) and high (I2 ≥ 75%) heterogeneity[13].
Subgroup analysis
A subgroup analysis was conducted to compare the predictors of early mortality based on the time interval between ACS onset and surgery. Specifically, studies were grouped into those where surgeries were performed within 24 h and those where surgeries were performed more than 24 h after ACS onset. Separate meta-analyses were conducted for each subgroup to identify and compare the predictors of early mortality. The same statistical methods used in the overall meta-analysis were applied to each subgroup.
Sensitivity analysis
To ensure the robustness of our findings, we performed a sensitivity analysis using the leave-one-out method for one of the risk factors. This analysis was carried out only for factors that included five or more studies. The goal of this analysis was to assess whether excluding a single study would significantly alter the overall results.
RESULTS
Search results and study characteristics
The initial search strategy identified 63 studies, of which 20 met the inclusion criteria and were incorporated into this meta-analysis [Table 1]. Five studies were prospective studies, while the rest of the studies were retrospective and observational in nature. The studies were conducted in various countries, including Israel, Japan, USA, Italy, Germany, Turkey, Singapore, and Vietnam. The types of acute coronary syndrome (ACS) included in these studies were STEMI, NSTEMI, and unstable angina (UA), with time to surgery ranging from ≤ 6 h to ≤ 72 h. All the studies included showed a low to moderate risk of bias, confirming the reliability of the combined data [Supplementary Table 1 and Supplementary Figure 1].
Patient demographics and baseline characteristics
The studies collectively included 4,777 patients who underwent emergency CABG within 72 h for ACS. The average age of patients ranged from 58 to 72 years, with a male predominance in all studies. Common comorbidities included hypertension (63%), diabetes mellitus (36%), hyperlipidemia (55%), and previous myocardial infarction (28%). The severity of coronary artery disease was quantified using the SYNTAX score, with most patients presenting with scores indicative of complex, multivessel disease.
Predictors of short-term mortality
The primary predictors of short-term mortality identified across the studies were advanced age, cardiogenic shock, chronic kidney disease, and preoperative intra-aortic balloon pump (IABP) [Table 2]. Pooled analysis showed that advanced age was significantly associated with increased short-term mortality (OR 1.40, 95%CI: 1.07-1.82, P = 0.01). Chronic kidney disease was another significant predictor, tripling the risk of short-term mortality (OR 3.19, 95%CI: 1.59-6.42, P = 0.001).
Meta-analysis of predictors of early mortality in ACS patients undergoing CABG
| Outcome | Studies | Participants (n = 4,777) | Statistical method | Effect estimate |
| Age | 6 | 1,255 | OR (IV, Random, 95%CI) | 1.40 [1.07, 1.82] |
| ·Female gender | 4 | 464 | OR (IV, Random, 95%CI) | 1.55 [0.61, 3.91] |
| Male gender | 4 | 674 | OR (IV, Random, 95%CI) | 0.46 [0.22, 0.94] |
| Cardiogenic shock | 7 | 1,099 | OR (IV, Random, 95%CI) | 5.35 [3.15, 9.09] |
| ·Diabetes | 5 | 569 | OR (IV, Random, 95%CI) | 1.66 [0.91, 3.06] |
| ·Dyslipidemia | 4 | 497 | OR (IV, Random, 95%CI) | 1.13 [0.40, 3.19] |
| ·Hypertension | 3 | 426 | OR (IV, Random, 95%CI) | 0.74 [0.34, 1.58] |
| ·Obesity | 2 | 359 | OR (IV, Random, 95%CI) | 1.03 [0.36, 2.95] |
| ·Neurological disease | 5 | 1,169 | OR (IV, Random, 95%CI) | 2.31 [0.92, 5.79] |
| CKD | 5 | 657 | OR (IV, Random, 95%CI) | 3.19 [1.59, 6.42] |
| ·COPD | 5 | 657 | OR (IV, Random, 95%CI) | 1.91 [0.57, 6.37] |
| ·PVD | 2 | 837 | OR (IV, Random, 95%CI) | 1.88 [0.29, 11.98] |
| IABP | 3 | 431 | OR (IV, Random, 95%CI) | 3.55 [1.30, 9.71] |
| ·LMS disease | 4 | 498 | OR (IV, Random, 95%CI) | 1.48 [0.75, 2.93] |
| ·LVEF < 30% | 3 | 684 | OR (IV, Random, 95%CI) | 2.46 [1.00, 6.04] |
| ·OPCAB | 11 | 2,254 | OR (IV, Random, 95%CI) | 0.72 [0.42, 1.25] |
Patients with preoperative IABP were found to have a significantly higher risk of mortality (OR 3.55, 95%CI: 1.30-9.71, P = 0.01). Cardiogenic shock was the strongest predictor of short-term mortality, with an OR of 5.35 (95%CI: 3.15-9.09, P < 0.00001). Male gender was identified as a protective factor against short-term mortality (OR 0.46, 95%CI: 0.22-0.94, P = 0.03).
Other factors such as female gender, diabetes, dyslipidemia, hypertension, obesity, neurological disease, chronic obstructive pulmonary disease, peripheral vascular disease, left main stem involvement, left ventricular ejection fraction < 30%, surgical approach (off-pump and on-pump) were also evaluated but did not reach statistical significance [Supplementary Figures 2-16].
Subgroup analysis
A subgroup analysis was conducted to assess predictors of early mortality in patients undergoing surgery for ACS based on the time interval between ACS onset and surgery. The analysis categorized studies into two groups: surgeries performed within 24 h of ACS onset and surgeries performed more than 24 h after ACS onset [Supplementary Table 2].
Age showed a consistent association with early mortality across all studies, with an overall odds ratio (OR) of 1.40 (95%CI: 1.07-1.82). Within subgroup analyses, the ORs for age were 1.62 (95%CI: 0.52-5.04) for surgeries within 24 h and 1.66 (95%CI: 0.86-3.23) for surgeries performed more than 24 h after ACS onset.
Gender analysis indicated that female gender did not exhibit a significant association with early mortality in either subgroup, with combined ORs of 1.55 (95%CI: 0.61-3.91), 2.93 (95%CI: 0.81-10.56) for surgeries within 24 h, and 0.77 (95%CI: 0.20-2.94) for surgeries performed more than 24 h after ACS onset. In contrast, male gender showed a protective effect overall (OR 0.46, 95%CI: 0.22-0.94), particularly pronounced within 24 h (OR 0.36, 95%CI: 0.13-0.97).
The presence of cardiogenic shock was consistently associated with higher mortality risk, with an overall OR of 5.35 (95%CI: 3.15-9.09). Subgroup analyses showed ORs of 6.21 (95%CI: 1.74-22.15) for surgeries within 24 h and 5.93 (95%CI: 3.14-11.19) for surgeries performed more than 24 h after ACS onset.
Diabetes, neurological disease, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), and other factors exhibited varying degrees of association with early mortality across subgroups. For instance, CKD demonstrated an OR of 3.19 (95%CI: 1.59-6.42) overall, with ORs of 1.88 (95%CI: 0.73-4.90) for surgeries within 24 h and 5.87 (95%CI: 2.10-16.38) for surgeries performed more than 24 h after ACS onset.
Off-pump coronary artery bypass (OPCAB) surgery showed an overall OR of 0.72 (95%CI: 0.42-1.25), with consistent findings across subgroups (ORs 0.78 within 24 h and 0.97 for surgeries performed more than 24 h after ACS onset).
These findings underscore the importance of considering the timing of surgery relative to ACS onset when assessing predictors of early mortality, highlighting differences in risk profiles and clinical outcomes based on this interval.
Sensitivity analysis
To assess the robustness of our findings, we conducted a Leave-One-Out Analysis, systematically excluding each study one at a time and re-running the meta-analysis [Supplementary Table 3]. The overall effect sizes and 95% confidence intervals remained mainly consistent across all iterations, apart from two notable changes in the CKD and OPCAB analyses. Excluding the Hirose study for CKD resulted in an overall effect size (OR) of 2.24 (95%CI: 0.99-5.09), indicating a reduction in the estimated risk compared to the initial analysis, which had an overall effect size of 3.19 (95%CI: 1.59-6.42). This suggests that the Hirose study had a significant impact on the higher initial risk estimation.
In the OPCAB analysis, removing the Locker study resulted in an overall effect size (OR) of 0.57 (95%CI: 0.36-0.90), demonstrating a more pronounced protective effect compared to the initial overall effect size of 0.72 (95%CI: 0.42-1.25). This indicates that the Locker study contributed to a more conservative estimation of the protective effect of OPCAB.
Excluding these studies provided a more robust and reliable estimation of the true effect size.
DISCUSSION
This systematic review and meta-analysis investigated predictors of short-term mortality in patients undergoing emergency CABG for ACS. The findings underscore several critical factors associated with early mortality, offering insights into risk stratification and perioperative management strategies.
Currently, PCI is the primary approach for managing patients with ACS, while CABG is mainly employed as a secondary treatment following initial medical and interventional management of myocardial infarction (MI)[14]. Approximately 5% of MI patients initially undergo CABG, with another 5% requiring salvage CABG due to failed angioplasty[15]. Emergency cardiac surgery in these cases is linked to high rates of morbidity and mortality, primarily due to infarcted area enlargement and hemorrhage[16].
Despite the undeniable significance of PCI in managing ACS, CABG remains crucial for a smaller subset of patients. Hwang et al. examined different CABG techniques - OPCAB, ONCAB, and on-pump beating heart CABG - in ACS patients[17]. The study noted OPCAB’s benefits in reducing risks such as stroke, renal failure, and prolonged ventilation compared to ONCAB, especially in emergency settings. The success of OPCAB, however, depends highly on surgical expertise and patient selection, with hemodynamic instability and technical challenges being significant predictors of short-term mortality.
Several studies have identified predictors of early mortality after emergency CABG. The timing of surgery post-MI is a significant predictor, with mortality rates reaching 15%-20% for patients operated on within the first 48 h post-MI, compared to 4%-5% for those who undergo surgery after 48 h[14,16].
Debate persists regarding the optimal timing for surgery after ACS. Myocardial revascularization aims to maintain myocardial function, prevent functional decline, and activate hibernating myocardium to boost ventricular function. These objectives advocate for timely revascularization. However, the study findings are heterogeneous. Bernard et al. recommended bypass grafting within a few days post-MI[18]. Conversely, Grothusen et al. suggested that 48 h is optimal for NSTEMI, noting no significant differences in mortality, ischemic recurrence, heart failure, or cardiogenic shock between the early and delayed intervention groups[19]. Daviewrwala et al. suggested a 24-h period for STEMI, while Assman et al. advocated a three-day delay for stable patients (both STEMI and NSTEMI)[20,21]. Parikh et al. reported high-risk patients revascularized within 48 h had similar mortality rates to those who waited longer[22]. A 2014 meta-analysis described a “U”-shaped curve for postoperative mortality, indicating low-risk patients benefit from early surgery, whereas high-risk patients should delay surgery to optimize recovery[16]. This evidence supports tailoring surgery timing based on individual risk profiles.
Our study identified advanced age, cardiogenic shock, CKD, and preoperative IABP as significant predictors of short-term mortality following emergency CABG. Advanced age emerged as a consistent predictor across all analyses, reinforcing its role as a crucial determinant of postoperative outcomes. This finding underscores the importance of careful patient selection and risk assessment, particularly in elderly ACS patients requiring urgent revascularization.
The presence of cardiogenic shock was identified as the strongest predictor of early mortality, with patients experiencing a five-fold increase in mortality risk compared to those without this complication. This underscores the critical need for rapid intervention and optimized hemodynamic management in these high-risk patients. Similarly, CKD was associated with a three-fold increase in mortality risk, highlighting the impact of renal function on perioperative outcomes in ACS patients undergoing emergency CABG. Conversely, male gender was found to have a protective effect against short-term mortality.
The identification of these predictors has significant clinical implications for risk stratification and perioperative management in ACS patients undergoing emergency CABG. Tailoring interventions based on individual risk profiles, such as optimizing preoperative renal function and managing cardiogenic shock, could potentially improve outcomes and reduce mortality rates.
Strengths and limitations
The strengths of our study include a comprehensive search strategy that adheres to PRISMA guidelines, rigorous quality assessment of included studies, and robust meta-analytical techniques to synthesize data across heterogeneous studies. Sensitivity and subgroup analyses further strengthened the robustness of our findings, demonstrating consistency across different patient cohorts and surgical timing intervals.
Limitations include inherent biases associated with retrospective and observational study designs, variations in study methodologies, and potential confounding factors not adjusted for in individual studies. Additionally, the exclusion of non-English studies may have introduced language bias, although efforts were made to minimize this through comprehensive database searches.
In conclusion, this systematic review and meta-analysis represent the first comprehensive analysis of predictors of short-term mortality following emergency CABG in patients with ACS. Our findings underscore the critical role of advanced age, cardiogenic shock, chronic kidney disease, and preoperative intra-aortic balloon pump as significant determinants of early mortality in this high-risk cohort. These results provide valuable insights into risk stratification and emphasize the need for tailored perioperative management strategies to enhance outcomes. Moving forward, continued research is essential to validate these findings across diverse patient populations and refine clinical guidelines for optimizing emergency CABG outcomes in ACS patients.
DECLARATIONS
Authors’ contributions
Conception and design: Comanici M, Raja SG
Data acquisition, analysis and interpretation, drafting the manuscript: Comanici M, Nadia B
Critical revision and supervision: Raja SG
All authors contributed to the conception, design, data acquisition, analysis, and interpretation of the study. All authors critically revised the manuscript and approved the final version.
Availability of data and materials
The data supporting the findings of this study are available within the article and its supplementary materials. Further data are available from the corresponding author upon reasonable request.
Financial support and sponsorship
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
Shahzad G. Raja is an Editorial Board member of the journal Vessel Plus, while the other authors have declared that they have no conflicts of interest.
Ethical approval and consent to participate
Ethical approval for this study was not necessary.
Consent for publication
Not applicable as this manuscript does not contain any individual person’s data.
Copyright
© The Author(s) 2024.
Supplementary Materials
REFERENCES
2. Möckel M. The new ESC acute coronary syndrome guideline and its impact in the CPU and emergency department setting. Herz. 2024;49:185-9.
3. Brown AJ, Ha FJ, Michail M, West NEJ. Prehospital diagnosis and management of acute myocardial infarction. In: Watson TJ, Ong PJL, Tcheng JE, editors. Primary angioplasty: a practical guide. Singapore: Springer; 2018. p. 15-29
4. Kofoed KF, Kelbæk H, Hansen PR, et al. Early versus standard care invasive examination and treatment of patients with non-ST-segment elevation acute coronary syndrome: VERDICT randomized controlled trial. Circulation. 2018;138:2741-50.
5. Surve TA, Kazim MA, Sughra M, et al. Revascularization modalities in acute coronary syndrome: a review of the current state of evidence. Cureus. 2023;15:e47207.
6. Neumann F-J, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165.
7. Shi WY, Smith JA, Shi WY, Smith JA. Role of coronary artery bypass surgery in acute myocardial infarction. In: Watson TJ, Ong PJL, Tcheng JE, editors. Primary angioplasty: a practical guide. Singapore: Springer; 2018. Chapter 16.
8. Horan PG, Leonard N, Herity NA. Progressively increasing operative risk among patients referred for coronary artery bypass surgery. Ulster Med J. 2006;75:136.
9. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 2021;372:n71.
10. Higgins JPT, Altman DG, Gøtzsche PC, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. Bmj. 2011;343:d5928.
11. Jpt H. Cochrane handbook for systematic reviews of interventions. Available from: https://dariososafoula.wordpress.com/wp-content/uploads/2017/01/cochrane-handbook-for-systematic-reviews-of-interventions-2019-1.pdf. [Last accessed on Sep 20].
13. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327:557-60.
14. Biancari F, Onorati F, Rubino AS, et al. Outcome of emergency coronary artery bypass grafting. J Cardiothorac Vasc Anesth. 2015;29:275-82.
15. Caceres M, Weiman DS. Optimal timing of coronary artery bypass grafting in acute myocardial infarction. Ann Thorac Surg. 2013;95:365-72.
16. Chen H-L, Liu K. Timing of coronary artery bypass graft surgery for acute myocardial infarction patients: a meta-analysis. Int J Cardiol. 2014;177:53-6.
17. Hwang B, Williams ML, Tian DH, Yan TD, Misfeld M. Coronary artery bypass surgery for acute coronary syndrome: a network meta‐analysis of on‐pump cardioplegic arrest, off-pump, and on-pump beating heart strategies. J Card Surg. 2022;37:5290-9.
18. Bernard C, Morgant MC, Jazayeri A, et al. Optimal timing of coronary artery bypass grafting in haemodynamically stable patients after myocardial infarction. Biomedicines. 2023;11:979.
19. Grothusen C, Friedrich C, Loehr J, et al. Outcome of stable patients with acute myocardial infarction and coronary artery bypass surgery within 48 h: a single-center, retrospective experience. J Am Heart Assoc. 2017;6:e005498.
20. Davierwala PM, Verevkin A, Leontyev S, Misfeld M, Borger MA, Mohr FW. Does timing of coronary artery bypass surgery affect early and long-term outcomes in patients with non–ST-segment–elevation myocardial infarction? Circulation. 2015;132:731-40.
21. Assmann A, Boeken U, Akhyari P, Lichtenberg A. Appropriate timing of coronary artery bypass grafting after acute myocardial infarction. Thorac Cardiovasc Surg. 2012;60:446-51.
22. Parikh SV, de Lemos JA, Jessen ME, et al. Timing of in-hospital coronary artery bypass graft surgery for non–ST-segment elevation myocardial infarction patients: results from the National Cardiovascular Data Registry ACTION Registry–GWTG (Acute coronary treatment and intervention outcomes network registry–get with the guidelines). JACC Cardiovasc Interv. 2010;3:419-27.
23. Locker C, Shapira I, Paz Y, et al. Emergency myocardial revascularization for acute myocardial infarction: survival benefits of avoiding cardiopulmonary bypass. Eur J Cardiothorac Surg. 2000;17:234-8.
24. Hirose H, Amano A, Takahashi A, Takanashi S. Urgent off-pump coronary artery bypass grafting. Jpn J Thorac Cardiovasc Surg. 2002;50:330-7.
25. Ochi M, Hatori N, Saji Y, Sakamoto S, Nishina D, Tanaka S. Application of off-pump coronary artery bypass grafting for patients with acute coronary syndrome requiring emergency surgery. Ann Thorac Cardiovasc Surg. 2003;9:29-35.
26. Kerendi F, Puskas JD, Craver JM, et al. Emergency coronary artery bypass grafting can be performed safely without cardiopulmonary bypass in selected patients. Ann Thorac Surg. 2005;79:801-6.
27. Onorati F, Feo M De, Mastroroberto P, et al. Unstable angina and non-ST segment elevation: surgical revascularization with different strategies. Eur J Cardio-Thorac. 2005;27:1043-50.
28. Thielmann M, Massoudy P, Neuhäuser M, et al. Prognostic value of preoperative cardiac troponin I in patients undergoing emergency coronary artery bypass surgery with non–ST-elevation or ST-elevation acute coronary syndromes. Circulation. 2006;114:I448-53.
29. Darwazah AK, Sham’a RAHA, Isleem I, Hanbali B, Jaber B. Off-pump coronary artery bypass for emergency myocardial revascularization. Asian Cardiovasc Thorac Ann 2009;17:133–8
30. Kaya K, Cavolli R, Telli A, et al. Off-pump versus on-pump coronary artery bypass grafting in acute coronary syndrome: a clinical analysis. J Cardiothorac Surg. 2010;5:31.
31. Joskowiak D, Szlapka M, Kappert U, Matschke K, Tugtekin SM. Intra-aortic balloon pump implantation does not affect long-term survival after isolated CABG in patients with acute myocardial infarction. Thorac Cardiovasc Surg. 2011;59:406-10.
32. Martinez EC, Emmert MY, Thomas GN, Emmert LS, Lee CN, Kofidis T. Off-pump coronary artery bypass is a safe option in patients presenting as emergency. Available from: https://www.zora.uzh.ch/id/eprint/42291/12/Martinez.pdf. [Last accessed on Sep 20].
33. Fattouch K, Runza G, Moscarelli M, et al. Graft patency and late outcomes for patients with ST-segment elevation myocardial infarction who underwent coronary surgery. Perfusion. 2011;26:401-8.
34. Sezai A, Hata M, Yoshitake I, et al. Results of emergency coronary artery bypass grafting for acute myocardial infarction: importance of intraoperative and postoperative cardiac medical therapy. Ann Thorac Cardiovasc Surg. 2012;18:338-46.
35. Khaladj N, Bobylev D, Peterss S, et al. Immediate surgical coronary revascularisation in patients presenting with acute myocardial infarction. J Cardiothorac Surg. 2013;8:1-7.
36. Hata M, Shiono M, Sezai A, et al. Outcome of emergency conventional coronary surgery for acute coronary syndrome due to left main coronary disease. Available from: https://www.researchgate.net/profile/Akira-Sezai/publication/7207495_Outcome_of_emergency_conventional_coronary_surgery_for_acute_coronary_syndrome_due_to_left_main_coronary_disease/links/0fcfd510886a7b598b000000/Outcome-of-emergency-conventional-coronary-surgery-for-acute-coronary-syndrome-due-to-left-main-coronary-disease.pdf [Last accessed on Sep 20].
37. Gaudino M, Glineur D, Mazza A, et al. Long-term survival and quality of life of patients undergoing emergency coronary artery bypass grafting for postinfarction cardiogenic shock. Ann Thorac Surg. 2016;101:960-6.
38. Davierwala PM, Leontyev S, Verevkin A, et al. Temporal trends in predictors of early and late mortality after emergency coronary artery bypass grafting for cardiogenic shock complicating acute myocardial infarction. Circulation. 2016;134:1224-37.
39. Hung DQ, Minh NT, Vo H-L, Hien NS, Tuan NQ. Impact of pre-, intra-and post-operative parameters on in-hospital mortality in patients undergoing emergency coronary artery bypass grafting: a scarce single-center experience in resource-scare setting. Vasc Health Risk Manag. 2021;17:211-26.
40. Bianchi G, Zancanaro E, Margaryan R, et al. Outcomes of emergent isolated coronary bypass grafting in heart failure patients. Life. 2022;12:2124.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Special Topic
Copyright
Data & Comments
Data


















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at [email protected].