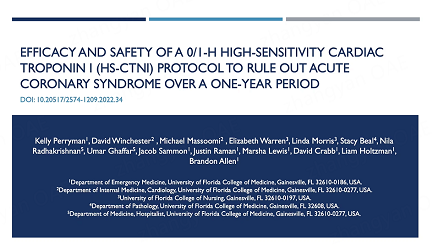
Efficacy and safety of a 0/1-h high-sensitivity cardiac troponin I (hs-cTnI) protocol to rule out acute coronary syndrome over a one-year period
Abstract
Aim: Evaluate the diagnostic and prognostic performance of the ESC 0/1H Algorithm and its utility in safely discharging patients with suspected Acute Coronary Syndrome (ACS) in the Emergency Department.
Methods: This analysis is a retrospective cohort study of 3,156 patients presenting to an academic medical center emergency department (ED) between May 20, 2019 and May 31, 2020. After completing the Beckman Coulter Access High Sensitivity Troponin I (hs-TnI) assay per current institution protocol (T0, T1H, T3H), patients identified to have symptoms concerning ACS were retrospectively analyzed using the ESC 0/1H Algorithm to assess the safety and efficacy of a rule-out algorithm for early discharge.
Results: The negative predictive value (NPV) of the protocol (T0 < 6 pg/mL; or females with T0 ≤ 15 pg/mL and
Conclusion: The protocol was found to have a NPV greater than 99% and a negative likelihood ratio of 0.08, suggesting it is safe to use for patients presenting to the ED with ACS symptoms no matter the time of symptom onset.
Keywords
INTRODUCTION
Myocardial infarction (MI) is a condition affecting 790,000 patients each year in the United States alone[1]. Acute myocardial injury (AMI) presentations account for up to 10% of total emergency department visits, and over 1 million annual hospital discharges are related to the diagnosis of coronary artery disease (CAD)[2,3]. Having the capability to rapidly and accurately diagnose ACS is paramount to early and effective initiation of guideline-directed management[4].
The current (fourth) Universal Definition of MI Expert Consensus Document updates the previous definition to accommodate the increased use of high-sensitivity cardiac troponin (hs-cTn) and includes acute myocardial injury (AMI)[5]. These assays have higher precision at low concentrations and are considered much more sensitive, enabling the development of standardized diagnostic approaches for ACS and acute versus chronic myocardial injury. However, widespread adoption of hs-cTn has been limited by concerns of reduced specificity.
Whereas Canada and countries in Europe and Asia have studied high-sensitivity troponin I and T (hs-cTnI and hs-cTnT, respectively) clinically for many years, the United States’ more recent adoption means hs-cTn characterization studies, such as cutoff determination for ruling-in or -out ACS and specifically AMI, are needed to understand the clinical implications in these populations[6-8].
The European Society of Cardiology’s most recent update to its 0/1h-algorithm extends the number of patients eligible for triage towards rule-out of AMI to those with low hs-cTnT/I concentrations at presentation and NO relevant change (rise AND/OR fall) in hs-cTnT/I concentrations after 1h. “The 2020 guidelines of the European Society of Cardiology (ESC) for the first time also recommended a novel ESC
Current recommendations for high-sensitivity cardiac troponin-I (hs-cTnI) assays include serial testing at
Our academic medical center is the first hospital system to implement the Beckman Coulter hs-TnI assay in the United States. Using this assay, our study aims to determine whether an early rule-out pathway based on the ESC 0/1-h algorithm could be used to safely discharge patients presenting to the ED with symptoms concerning ACS.
Background
Of all patients who present to EDs with ACS symptoms, less than 10% experience myocardial infarction[19,20]. Though most patients presenting with ACS symptoms do not have AMI, evaluation of these patients can result in costly imaging and monitoring, long hospital stays, and unnecessary hospital admissions[19]. While it is crucial not to miss a cardiac diagnosis, not every rule out ACS patient can be admitted due to limited resources and risks associated with hospitalization. This leaves the healthcare system with a pressing need for safe and effective early AMI rule-out protocols[21]. An economic analysis by Shortt et al. found that early AMI rule-out protocols can benefit both patients and the healthcare system. They compared costs between the utilization of different lab tests (cTnI, hs-cTnI, hs-cTnT, glucose, and/or hemoglobin A1C) for ruling out AMI in the ED and found that algorithms incorporating hs-cTnI for early rule-out were the most cost effective, despite the initial extra cost for hs-cTnI tests[22]. A stepped-wedge cluster randomized controlled trial found that an early rule-out hs-cTnI protocol reduced the length of hospital stays by an average of 3.3 h and the chance of hospital re-admission by 59%[23,24]. Another analysis suggested the overall reduction in economic costs of using a 1-h algorithm compared to standard of care (SOC) are in the range of 30-46%[25].
Despite the immense need for early AMI rule-out protocols and consistent findings demonstrating safety and cost effectiveness, there has been slow adoption among EDs, due to fear of litigation in case of missed AMIs as well as previous studies which raised concerns about the generalizability of such protocols and recommended only applying them in low-risk populations[19,26]. Further, research on 0/1-h hs-cTnI protocols specifically has been lacking.
In the Emergency Department, early rule-out algorithms utilizing high-sensitivity troponin assays provide a way to rule-out AMI with an acceptable tradeoff between speed and safety. Such algorithms allow for improved diagnostic accuracy, timely treatment, and safe discharge.
METHODS
This retrospective cohort study was conducted at a single large academic medical center with an adult emergency department and two freestanding emergency departments. Upon implementation of the hs-TnI assay, this institution elected to use a T0, 1, and 3-h serial strategy. The subjects in this study were seen in the EDs between May 20, 2019 and May 31, 2020 with symptoms concerning acute coronary syndrome (ACS) and had a completed troponin series.
Assay
The Beckman Coulter Access High Sensitivity Troponin I (hsTnI) assay was implemented on the DxI 800 analyzer in the Core Laboratory and the Access analyzer in the free-standing emergency departments. This chemiluminescent sandwich immunoassay has a run time of approximately 15 min and is performed on 55 microliters of serum or plasma. According to the package insert, the Beckman Coulter hs-cTnI assay meets the two fundamental criteria of a “high-sensitivity” assay: (1) the assay is capable of measuring cTnI concentrations at or above the LoD in ≥ 50% of healthy individuals; (2) the error measurement corresponding to the 99th percentile is ≤ 10%[27-29].
The cutpoints were achieved through consensus of key stakeholders from the laboratory, ED, and cardiology, following review of the package insert for sex-specific cutpoints. The interpretation of hs-TnI was determined to be as follows: ≤ 15 pg/mL: within normal range for females; ≤ 20 pg/mL: within normal range for males; > 100 pg/mL: suspected acute myocardial injury; and for all other values: delta guidelines/algorithm will be used[27,28,30]. Researchers from our institution previously published a correlation study in the Journal of Applied Laboratory Medicine validating the institution’s cutpoints[30].
Exclusion criteria
An electronic heath record report was generated for the study period indicating ICD-10 codes for myocardial infarction (MI), ACS, or AMI and 30-day death. During the study period, there were 26,987 subjects seen at the UF Health ED who had a troponin level measured. 23,831 of those subjects were excluded because they did not have symptoms concerning for ACS, left against medical advice (AMA), left without being seen (LWBS), eloped, or were found to have STEMI at the index ED visit, leaving 3,156 subjects to be included in the analysis. Subjects were determined to have symptoms concerning for ACS if they met the following criteria: (1) chest pain was listed as their first complaint in the EMR; and (2) any secondary complaint was one of the ACS symptoms listed in the American College of Cardiology’s Chest Pain Accreditation Conformance Database (Version 7) except cardiac arrest which was excluded (i.e., abdominal pain/indigestion, arm pain, back/shoulder/scapula pain, confusion/altered mental status, diaphoresis, dizziness, fatigue/weakness, jaw pain, nausea/vomiting, palpitations, shortness of breath/dyspnea, or syncope). The process of inclusion and exclusion of study participants is shown in Figure 1.
Cohort assignment
Based on hs-TnI T0, 1h and delta results, the subjects were categorized into a rule-out, observation, or rule-in group. The rule-out group was comprised of those with hs-TnI T0 < 6 pg/mL or females T0 and 1h ≤ 15 pg/mL or males T0 and 1h ≤ 20 pg/mL. The observation group was comprised of females with hs-TnI T0 or 1h > 15 pg/mL and ≤ 100 pg/mL or males with hs-TnI T0 or 1h > 20 pg/mL and ≤ 100 pg/mL. The rule-in group was comprised of those with T0 or 1h >100 pg/mL or delta > 15 pg/mL.
Analysis
Manual chart adjudication was performed on subjects with myocardial infarction, ACS, or AMI ICD-10 coding to validate ACS. Adjudication was also performed for those with a 30-day death outcome by two separate adjudicators and a third if necessary to identify confirmed or suspected cardiac-related cause. Any unknown cause of death was considered cardiac-related.
A negative predictive value (NPV) of NSTEMI and 30-day death was calculated for subjects in the rule-out category. A positive predictive value (PPV) of NSTEMI and 30-day death was calculated for subjects in the rule-in category. Likelihood ratios (LRs) were calculated for all groups. Based on local policy, this was determined to be QI and not human subjects research and designated QIPR Project ID 1124.
RESULTS
Key demographics and characteristics of the subjects analyzed can be found below in Table 1. Based on the triage algorithm, 2,551/3,156 (81%) subjects were placed in the “rule-out” group, 347/3,156 (11%) were placed in the “observation” group, and 258/3,156 (8%) were placed in the “rule-in” group [Table 2]. The overall efficacy of the algorithm, defined by the proportion of subjects within either the “rule-in” or “rule-out” group, was 89%.
Subject demographics and characteristics
| n | 3157 |
| Females | 1591 (50.4%) |
| Median age years | 55 |
| Median BNP | 40 pg/mL |
| Median eGFR | 60 mL/min/1.73M2 |
| Median creatinine | 0.9 mg/dL |
| Troponin measurements met the definition of acute myocardial injury* | 307 (9.7%) |
| ED Disposition** | |
| To Home | 1568 (49.7%) |
| Observation | 405 (12.8%) |
| Inpatient | 1184 (37.5%) |
| Received Catheterization | 269 (8.5%) |
| Received Cardiology Consult*** | 511 (16.2%) |
Classification of 3,156 subjects by 0/1-h Algorithm using hs-cTnI
| Disease | Rule-out | Observation | Rule-in | Total |
| No AMI/30d Cardiac Death | 2536 | 318 | 84 | 2938 |
| AMI/30d Cardiac Death | 15 | 29 | 174 | 218 |
| Total | 2551 | 347 | 258 | 3156 |
The negative predictive value (NPV) of the protocol (T0 < 6 pg/mL; or females with T0 ≤ 15 pg/mL and
Within the “rule-out” group, there were 15/2,551 (0.6%) subjects who went on to experience one of the defined Major Adverse Cardiovascular Events (MACE) outcomes, with 9 (0.4%) having an index MI and 6 (0.2%) experiencing cardiac related-death within 30 days of index visit. These 15 subjects are further characterized below in Table 2. All 15 of these subjects were admitted, including one subject who left AMA after being accepted for admission but before being transitioned to inpatient care.
Table 3 provides an overview of the 15 subjects in the “rule-out” group who experienced index NSTEMI or 30-day cardiac-related death. The descriptions in the column titled “MACE” were derived from ICD-10 codes and chart review (rather than from troponin values), and they do not necessarily align with the definition of myocardial injury set by the Fourth Universal Definition of Myocardial Infarction (2018) of having an elevated cTnI above the 99th percentile[2]. Of the 15 subjects who were “ruled out” by the algorithm and went on to experience adverse outcomes, 7/15 (46.7%) met that definition[5]. Because the protocol utilized only the first two measurements (T0 and T1), subjects with two initial low troponins (T0 and T1) but a high troponin measured later during the index visit (e.g., T3) were “ruled out” by the protocol although “myocardial injury” was present according to the Fourth Universal Definition of Myocardial Infarction. Of those 7 subjects, 3 were “ruled out” after a single hs-TnI measurement (T0) and 4 were “ruled out” after two (T0 and T1). In all of these cases, the ED providers chose to admit them.
Characteristics of all 15 subjects in the “rule-out” group who experienced index NSTEMI or 30-day cardiac-related death
| MACE | Age | Race | Ethnicity | Sex | BMI> 30 | ECG at arrival | HEART score | Initial troponin value (pg/mL) | Troponin 1 hour value (pg/mL) | Troponin 3 hour value (pg/mL) | Max Δtroponin (pg/mL) | Met fourth definition of myocardial injury* | Acute vs. chronic myocardial injury** | ED disposition*** |
| Cardiac arrest secondary to HFrEF within 30 days | 60 | Black or AA | Non-Hispanic | Male | No | Non-ischemic | Not documented | 8 | 8 | 8 | 0 | No | Inpatient | |
| Death of unknown cause within 30 days (assume cardiac-related) | 79 | White | Non-Hispanic | Female | No | Non-ischemic | 7 | 6 | 6 | 7 | 1 | No | Inpatient | |
| STEMI within 30 days | 55 | Black or AA | Non-Hispanic | Male | No | Non-ischemic | Not documented | 13 | 11 | 8 | 5 | No | Inpatient | |
| Death of unknown cause within 30 days (assume cardiac-related) | 66 | White | Non-Hispanic | Male | No | Non-ischemic | Not documented | 17 | 16 | N/A | 1 | No | Observation | |
| Death of unknown cause within 30 days (assume cardiac-related) | 49 | Black or AA | Non-Hispanic | Female | Yes | Ischemic | 5 | 14 | 13 | 15 | 2 | No | Decision to Admit**** | |
| Complete heart block and septic shock secondary to endocarditis within 30 days | 72 | White | Non-Hispanic | Male | No | Non-ischemic | Not documented | 17 | 19 | 19 | 2 | No | Inpatient | |
| NSTEMI (occluded PDA; no targets for revascularization in recent left heart catheterization) | 68 | Black or AA | Non-Hispanic | Male | No | Non-ischemic | 5 | 5 | 5 | 11 | 6 | No | Inpatient | |
| NSTEMI, type II | 81 | White | Non-Hispanic | Female | No | Non-ischemic | 6 | 15 | 15 | 15 | 0 | No | Observation | |
| NSTEMI | 62 | White | Non-Hispanic | Male | Yes | Non-ischemic | Not documented | 12 | 18 | 237 | 225 | Yes | Acute | Inpatient |
| NSTEMI | 38 | White | Non-Hispanic | Female | Yes | Non-ischemic | 4 | 10 | 15 | 33 | 23 | Yes | Acute | Inpatient |
| NSTEMI | 67 | White | Non-Hispanic | Male | Yes | Non-ischemic | Not documented | 10 | 14 | 34 | 24 | Yes | Acute | Inpatient |
| NSEMI (cath showed CAD with high-grade stenosis of mid LAD and moderate disease in mid RCA) | 52 | White | Non-Hispanic | Male | No | Non-ischemic | 5 | 12 | 20 | 27 | 15 | Yes | Chronic | Inpatient |
| NSTEMI | 75 | White | Non-Hispanic | Female | No | Non-ischemic | Not documented | 5 | 7 | 121 | 116 | Yes | Acute | Observation |
| NSTEMI, type II | 43 | White | Non-Hispanic | Female | No | Non-ischemic | 2 | 5 | 11 | 77 | 72 | Yes | Acute | Inpatient |
| NSTEMI | 71 | Black or AA | Non-Hispanic | Female | Yes | Non-ischemic | 7 | 5 | 7 | 31 | 26 | Yes | Acute | Inpatient |
According to the Fourth Universal Definition of Myocardial Infarction (2018), “the term myocardial injury should be used when there is evidence of elevated cardiac troponin values (cTn) with at least one value above the 99th percentile upper reference limit (URL)...the term acute myocardial injury should be used when there is acute myocardial injury with evidence of acute myocardial ischemia and with detection of a rise and/or fall of cTn values...”[5]. In this analysis, a “significant rise and/or fall of cTn values” was defined as a change in cTn greater than 15 pg/mL (delta 1h > 15 pg/mL). Myocardial injury was designated “acute myocardial injury” if delta 1h > 15 pg/mL and “chronic myocardial injury” if delta 1h ≤ 15 pg/mL [Table 2].
DISCUSSION
In this retrospective cohort study, we evaluated a 0,1-h hs-cTnI protocol for ruling out AMI among patients presenting to an academic health center ED with ACS symptoms over a one-year period. The protocol was found to have an NPV greater than 99% and negative likelihood ratio of 0.08, suggesting it is safe to use for patients presenting to the ED with ACS symptoms no matter the time of symptom onset. Though the pre-test probability of AMI has a median prevalence of 12% across studies[31], the negative likelihood ratio of the protocol is sufficiently low that the post-test probability of AMI would be low despite a higher pre-test probability[32]. Because our analysis yielded a high NPV in a broad, diverse population of 3,156 patients over a year-long period, it is reasonable to generalize the findings.
Upon review of the literature, there has not been a previous analysis of the efficacy of the 0,1-h hs-cTnI protocol using the Beckman Coulter assay in a patient population of this size. The findings provide evidence of the efficacy and safety of the protocol using the Beckman Coulter hs-cTnI assay to rule out AMI, for application in other EDs.
When implementing such a protocol at other institutions, it is of utmost importance to use the cut-offs recommended for the assay being used, as cutoffs are assay-specific and vary significantly[33]. Failure to do so could decrease the NPV of the protocol, resulting in patients with AMI being incorrectly “ruled-out” and reducing safety of the protocol.
In our analysis, only 6.9% of the patients who presented to the UF Health EDs with ACS symptoms over a one-year period experienced index NSTEMI or 30 day cardiac-related death based on ICD-codes and adjudication. This is consistent with many studies of early myocardial infarction rule-out protocols which have less than 10% of patients with MI[20]. The literature substantiates our results that support the safety of a 0,1-h hs-cTnI protocol. The high NPV of our analysis is consistent with the results of multiple previous studies of early rule-out hs-cTnI protocols, which also had NPVs greater than 99%[14,15,34-36]. Additionally, several studies have shown safety of a 0,1-h hs-cTnT protocol, providing further evidence of the safety of a 0,1-h hs-cTn protocol in general[32,37-39]. The 2020 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-Elevation recommends using a 0/1-h or 0/2-h hs-cTnI algorithm for ruling out AMI[11]. Anand et al. also found that an early rule-out hs-cTnI protocol reduced hospital admissions and length of hospital stays without a difference in hospital readmission or all-cause mortality[23]. The high NPVs of this analysis and others evaluating 0/1-h hs-cTnI protocols suggests that such a protocol may be safely applied at other institutions.
Safety of a 0,1-h protocol using hs-cTnT has been shown in populations of over 3,000 patients in multiple studies but not using hs-cTnI[26,40,41]. Our study expands on prior studies of 0,1-h hs-cTnI protocols performed with smaller samples, allowing for greater generalizability of the findings[14,16,34]. Further, few prior studies have specifically evaluated the protocol using the Beckman Coulter Access High Sensitivity Troponin I (hsTnI) assay.
Further studies examining the cutoff values for early rule-out hs-cTn protocols may be warranted. Of note, 3/15 (0.2%) of the subjects who were “ruled-out” by the protocol but went on to experience AMI or 30d cardiac death were “ruled-out” based on borderline troponin values. In other words, if the cutoff levels had been decreased by one, these subjects would have been placed in the “observation” group, increasing the NPV of the protocol. Further, Sandoval et al. found that individuals with an undetectable troponin level (hs-cTnT<3) had similar risk of incident atherosclerotic cardiovascular disease (ASCVD) as those with a coronary artery calcium (CAC) of zero[42]. This suggests that small changes in high-sensitivity troponin may be significant at low levels, supporting the need for careful determination of cutoff levels.
Despite its high NPV, the protocol should be applied in combination with provider judgement for optimal safety. Boeddinghaus et al. recommends that in addition to an early rule-out hs-TnI protocol, patients presenting with chest pain should first have an ECG to rule-out STEMI, followed by evaluation with repeat ECG, history (including chest pain characteristics), physical exam, and troponin measurement at 3 h when clinical decision-making suggests AMI[14]. Additionally, they emphasize that not every patient ruled out by such a protocol can be discharged, depending on other conditions present[14]. Twerenbold et al. recommends that optimal usage of hs-cTnI/T assays is with a rapid rule-out algorithm and within the context of an institutional standard operating procedure[43]. In this analysis, the protocol incorrectly placed 15/2,551 (0.6%) subjects in the “rule-out” group (these patients went on to experience AMI and/or 30-day cardiac death). Despite the protocol placing these patients in the “rule-out” group, the ED providers appropriately made the decision to admit all 15 of these patients.
The 2020 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-Elevation recommends that the minimum PPV for a rule-in strategy should be 70%[11]. Though the PPV of this protocol was 67.4% and not high enough to justify using it as a standalone diagnostic tool, further research is warranted on the use of 0/1-h protocols for rule-in.
Of those subjects placed in the “observation” group in our analysis, 29/347 (8.4%) went on to experience one of the defined adverse events. This was low relative to the “rule-in” group, in which 174/258 (67.4%) experienced one of the defined adverse events, and high relative to the “rule-out” group, in which 15/2551 (0.6%) experienced one of the defined adverse events. Gimenez et al. recommends that treatment of patients in the “observation” group of early rule-out protocols varies significantly and must be tailored to individuals rather than standardized[36]. Some studies of early rule-out protocols have found significantly higher incidence of NSTEMI in the “observation” group, supporting the need for careful, individualized assessment in this group[44]. Further studies are warranted to better understand and evaluate this group.
There are several limitations of this analysis which should be considered when interpreting its findings. First, our analysis examined patients seen only at a single academic health center, limiting generalizability of the results. Second, the study was a retrospective analysis, which are susceptible to selection and information biases and can be affected by missing data. Examination of the question with other study designs, such as prospective analysis, is warranted. Third, ICD-10 diagnosis codes were used to determine outcomes, and any missing or incorrectly entered ICD-10 codes would have affected the results. Fourth, there was no known follow-up outside the single health system, so there is the possibility of unaccounted events occurring at other facilities. Of note, due to the nature of medical record systems, we believe it would be more likely for an event such as an NSTEMI to occur and not make it into our records relative to a death, which would likely be reported to our health system. In conclusion, the 0/1-h cTnI protocol is a safe and effective option for early AMI rule-out that can facilitate quicker discharge of ACS patients in the ED.
In conclusion, in this single-center analysis where the Beckman hs-cTnI assay was implemented first in the United States, a 0/1h protocol with this assay was identified as safe and efficacious to exclude acute myocardial injury. Utilization of similar protocols for patients with symptoms concerning for ACS should be considered for widespread use.
DECLARATIONS
Authors’ contributionsConceived and designed the analysis: Allen B, Warren E
Collected the data: Perryman K, Allen B, Warren E, Sammon J, Raman J
Performed the analysis: Perryman K, Allen B, Warren E, Sammon J, Raman J
Wrote the paper: Perryman K, Allen B, Warren E, Sammon J, Raman J
Other contribution: Winchester D
Reviewed the final manuscript: All authors
Availability of data and materialsData obtained from electronic medical record system.
Financial support and sponsorshipNone.
Conflicts of interestDr. Allen B. receives research funding/support from Roche Diagnostics, Siemens and Beckman Coulter. He is a consultant for Roche Diagnostics. Dr. Winchester D. is supported by Career Development Award #13-023 from the United States Department of Veterans Affairs Health Services Research and Development Service. Other authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2023.
REFERENCES
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the american heart association. Circulation 2017;135:e146-603.
2. Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the american heart association. Circulation 2021;143:e254-743.
3. Boeddinghaus J, Twerenbold R, Nestelberger T, et al. Clinical validation of a novel high-sensitivity cardiac troponin I assay for early diagnosis of acute myocardial infarction. Clin Chem 2018;64:1347-60.
4. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;130:e344-426.
5. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction. J Am Coll Cardiol 2018;72:2231-64.
6. Tan JWC, Lam CSP, Kasim SS, et al. Asia-Pacific consensus statement on the optimal use of high-sensitivity troponin assays in acute coronary syndromes diagnosis: focus on hs-TnI. Heart Asia 2017;9:81-7.
7. Nowak RM, Christenson RH, Jacobsen G, et al. Performance of novel high-sensitivity cardiac troponin i assays for 0/1-hour and 0/2- to 3-hour evaluations for acute myocardial infarction: results from the HIGH-US study. Ann Emerg Med 2020;76:1-13.
8. Thygesen K, Mair J, Giannitsis E, et al. How to use high-sensitivity cardiac troponins in acute cardiac care. Eur Heart J 2012;33:2252-7.
9. Koechlin L, Boeddinghaus J, Nestelberger T, et al. Performance of the ESC 0/2h-algorithm using high-sensitivity cardiac troponin I in the early diagnosis of myocardial infarction. Am Heart J 2021;242:132-7.
10. Boeddinghaus J, Reichlin T, Cullen L, et al. Two-hour algorithm for triage toward rule-out and rule-in of acute myocardial infarction by use of high-sensitivity cardiac troponin I. Clin Chem 2016;62:494-504.
11. Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289-367.
12. Twerenbold R, Neumann JT, Sörensen NA, et al. Prospective validation of the 0/1-h algorithm for early diagnosis of myocardial infarction. J Am Coll Cardiol 2018;72:620-32.
13. Boeddinghaus J, Nestelberger T, Koechlin L, et al. Early diagnosis of myocardial infarction with point-of-care high-sensitivity cardiac troponin I. J Am Coll Cardiol 2020;75:1111-24.
14. Boeddinghaus J, Twerenbold R, Nestelberger T, et al. Clinical use of a new high-sensitivity cardiac troponin I assay in patients with suspected myocardial infarction. Clin Chem 2019;65:1426-36.
15. Boeddinghaus J, Nestelberger T, Twerenbold R, et al. High-sensitivity cardiac troponin I assay for early diagnosis of acute myocardial infarction. Clin Chem 2019;65:893-904.
16. Cook B, McCord J, Hudson M, et al. Baseline high sensitivity cardiac troponin I level below limit of quantitation rules out acute myocardial infarction in the emergency department. Crit Pathw Cardiol 2021;20:4-9.
17. Kontos MC, Turlington JS. High-sensitivity troponins in cardiovascular disease. Curr Cardiol Rep 2020;22:30.
18. Allen BR, Christenson RH, Cohen SA, et al. Diagnostic performance of high-sensitivity cardiac troponin T strategies and clinical variables in a multisite US cohort. Circulation 2021;143:1659-72.
19. Chapman AR, Anand A, Boeddinghaus J, et al. Comparison of the efficacy and safety of early rule-out pathways for acute myocardial infarction. Circulation 2017;135:1586-96.
20. Morrow DA. Clinician’s guide to early rule-out strategies with high-sensitivity cardiac troponin. Circulation 2017;135:1612-6.
21. Januzzi JL Jr, McCarthy CP. Evaluating chest pain in the emergency department: searching for the optimal gatekeeper. J Am Coll Cardiol 2018;71:617-9.
22. Shortt C, Xie F, Whitlock R, et al. Economic considerations of early rule-in/rule-out algorithms for the diagnosis of myocardial infarction in the emergency department using cardiac troponin and glycemic biomarkers. Clin Chem 2017;63:593-602.
23. Anand A, Lee KK, Chapman AR, et al. High-sensitivity cardiac troponin on presentation to rule out myocardial infarction: a stepped-wedge cluster randomized controlled trial. Circulation 2021;143:2214-24.
24. Jülicher P, Greenslade JH, Parsonage WA, Cullen L. The organisational value of diagnostic strategies using high-sensitivity troponin for patients with possible acute coronary syndromes: a trial-based cost-effectiveness analysis. BMJ Open 2017;7:e013653.
25. Ambavane A, Lindahl B, Giannitsis E, et al. Economic evaluation of the one-hour rule-out and rule-in algorithm for acute myocardial infarction using the high-sensitivity cardiac troponin T assay in the emergency department. PLoS One 2017;12:e0187662.
26. Stoyanov KM, Hund H, Biener M, et al. RAPID-CPU: a prospective study on implementation of the ESC 0/1-hour algorithm and safety of discharge after rule-out of myocardial infarction. Eur Heart J Acute Cardiovasc Care 2020;9:39-51.
27. High-sensitivity* cardiac troponin I and T assay analytical characteristics designated by manufacturer IFCC committee on clinical applications of cardiac bio-markers (C-CB) V062019. Available from: https://ifcc.org/ifcc-education-division/emd-committees/committee-on-clinical-applications-of-cardiac-bio-markers-c-cb/biomarkers-reference-tables/ [Last accessed on 24 March 2023].
28. CDRH. 510(k) substantial equivalence determination decision memorandum assay only template. Available from: https://www.accessdata.fda.gov/cdrh_docs/reviews/K170200.pdf [Last accessed on 24 March 2023].
29. Wu AHB, Christenson RH, Greene DN, et al. Clinical laboratory practice recommendations for the use of cardiac troponin in acute coronary syndrome: expert opinion from the academy of the American association for clinical chemistry and the task force on clinical applications of cardiac bio-markers of the international federation of clinical chemistry and laboratory medicine. Clin Chem 2018;64:645-55.
30. Beal SG, Winchester DE, Wilkerson G, Harris N, Allen B. Comparison of patient results on a new high-sensitivity troponin I assay with a conventional assay, focusing on clinically relevant cutpoints. J Appl Lab Med 2020;5:597-9.
31. Chiang CH, Chiang CH, Pickering JW, et al. Performance of the European society of cardiology 0/1-hour, 0/2-hour, and 0/3-hour algorithms for rapid triage of acute myocardial infarction: an international collaborative meta-analysis. Ann Intern Med 2022;175:101-13.
32. Nilsson T, Johannesson E, Lundager Forberg J, Mokhtari A, Ekelund U. Diagnostic accuracy of the HEART Pathway and EDACS-ADP when combined with a 0-hour/1-hour hs-cTnT protocol for assessment of acute chest pain patients. Emerg Med J 2021;38:808-13.
33. Clerico A, Ripoli A, Zaninotto M, et al. Head-to-head comparison of plasma cTnI concentration values measured with three high-sensitivity methods in a large Italian population of healthy volunteers and patients admitted to emergency department with acute coronary syndrome: a multi-center study. Clin Chim Acta 2019;496:25-34.
34. Chapman AR, Fujisawa T, Lee KK, et al. Novel high-sensitivity cardiac troponin I assay in patients with suspected acute coronary syndrome. Heart 2019;105:616-22.
35. Reichlin T, Twerenbold R, Wildi K, et al. Prospective validation of a 1-hour algorithm to rule-out and rule-in acute myocardial infarction using a high-sensitivity cardiac troponin T assay. CMAJ 2015;187:E243-52.
36. Rubini Gimenez M, Twerenbold R, Jaeger C, et al. One-hour rule-in and rule-out of acute myocardial infarction using high-sensitivity cardiac troponin I. Am J Med 2015;128:861-870.e4.
37. Body R, Carley S, McDowell G, et al. Rapid exclusion of acute myocardial infarction in patients with undetectable troponin using a high-sensitivity assay. J Am Coll Cardiol 2011;58:1332-9.
38. Reichlin T, Schindler C, Drexler B, et al. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med 2012;172:1211-8.
39. Mokhtari A, Borna C, Gilje P, et al. A 1-h combination algorithm allows fast rule-out and rule-in of major adverse cardiac events. J Am Coll Cardiol 2016;67:1531-40.
40. Wereski R, Kimenai DM, Taggart C, et al. Cardiac troponin thresholds and kinetics to differentiate myocardial injury and myocardial infarction. Circulation 2021;144:528-38.
41. Chew DP, Lambrakis K, Blyth A, et al. A randomized trial of a 1-hour troponin T Protocol in suspected acute coronary syndromes: the rapid assessment of possible acute coronary syndrome in the emergency department with high-sensitivity troponin T study (RAPID-TnT). Circulation 2019;140:1543-56.
42. Sandoval Y, Bielinski SJ, Daniels LB, et al. Atherosclerotic cardiovascular disease risk stratification based on measurements of troponin and coronary artery calcium. J Am Coll Cardiol 2020;76:357-70.
43. Twerenbold R, Boeddinghaus J, Nestelberger T, et al. Clinical use of high-sensitivity cardiac troponin in patients with suspected myocardial infarction. J Am Coll Cardiol 2017;70:996-1012.
Cite This Article
How to Cite
Perryman K, Winchester D, Massoomi M, Warren E, Morris L, Beal S, Radhakrishnan N, Ghaffar U, Sammon J, Raman J, Lewis M, Crabb D, Holtzman L, Allen B. Efficacy and safety of a 0/1-h high-sensitivity cardiac troponin I (hs-cTnI) protocol to rule out acute coronary syndrome over a one-year period. Vessel Plus. 2023;7:7. http://dx.doi.org/10.20517/2574-1209.2022.34
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Copyright
Related
Data & Comments
Data






















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.