Reconstructive rhinoplasty for the contracted Asian nose
Abstract
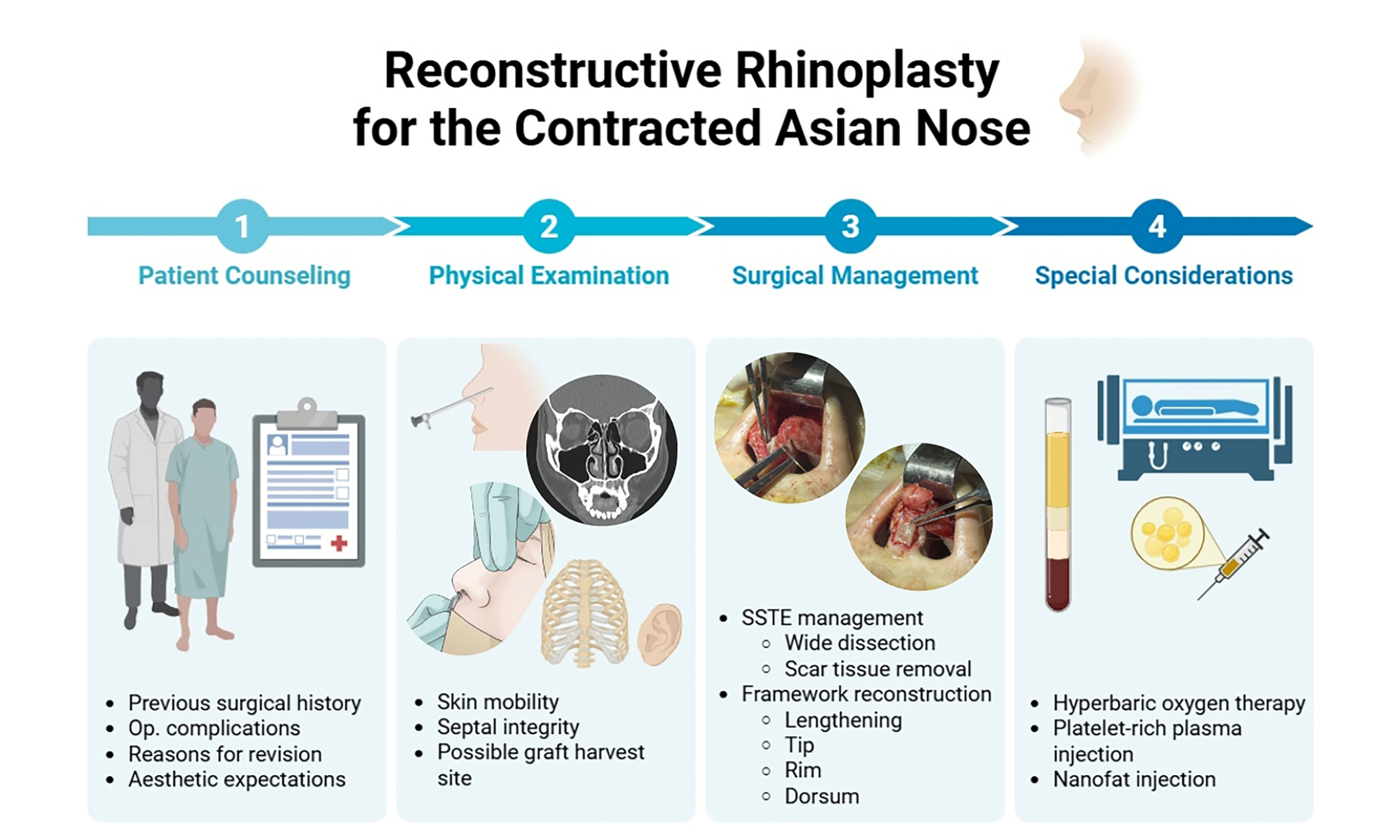
A contracted nose deformity is a challenging and distinct complication of rhinoplasty, particularly prevalent among Asian patients due to implant-related complications and infection-induced scar formation. Clinical presentations range from mild nasal tip upturning to severe distortion of nasal structures. This review outlines comprehensive surgical strategies for managing the contracted Asian nose, including wide release of the skin-soft tissue envelope, structural framework reconstruction with autologous rib cartilage, nasal tip elongation, and skin redraping techniques. Special considerations such as platelet-rich plasma, nanofat injection, and hyperbaric oxygen therapy are also discussed. Successful outcomes require meticulous planning, surgical expertise, and realistic patient expectations.
Keywords
INTRODUCTION
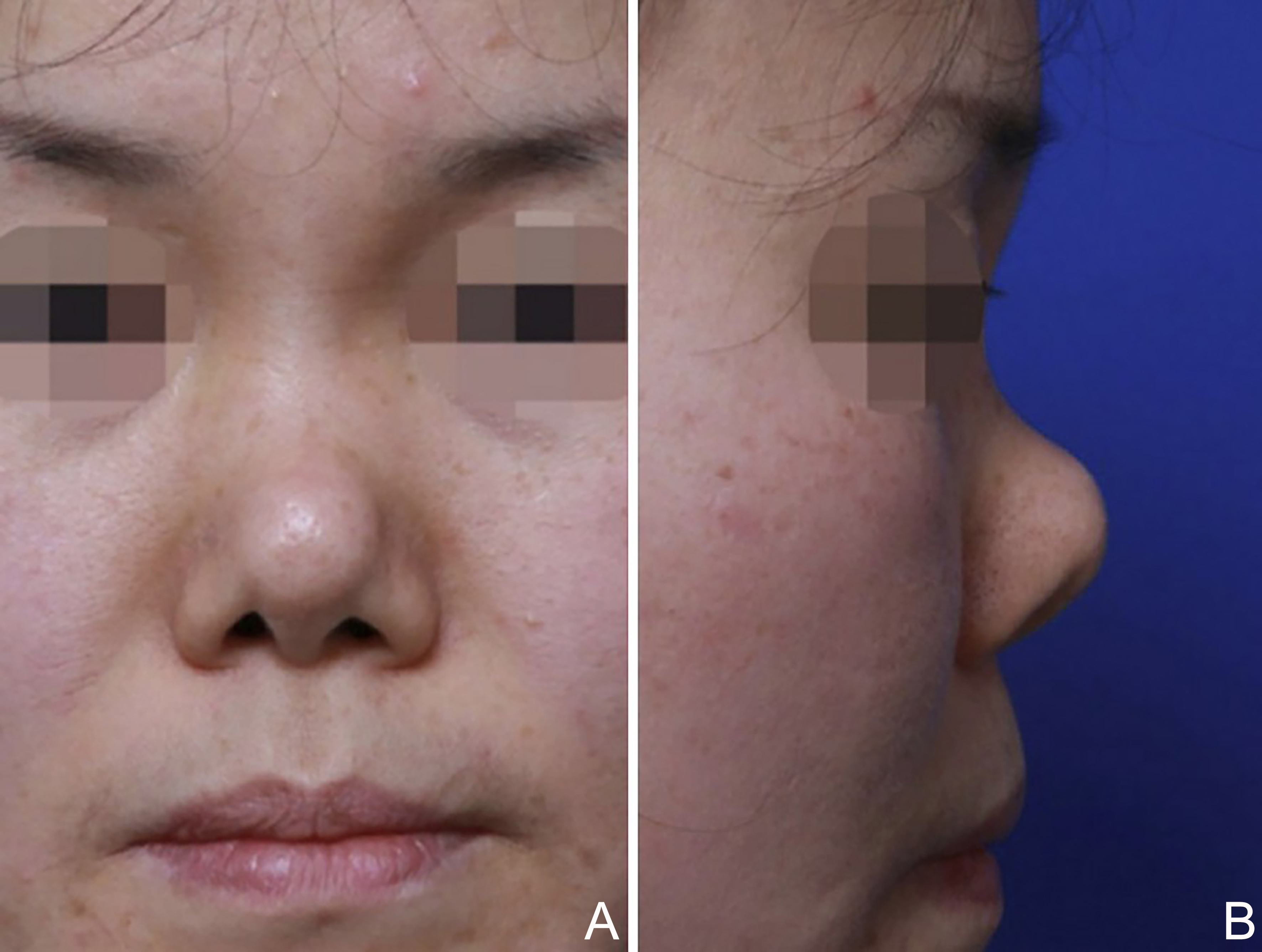
A contracted nose deformity is a distinct postoperative complication of rhinoplasty, particularly prevalent in Asian patients[1,2]. It presents in various forms, ranging from mild skin contracture with an upturned nasal tip to severe distortion of the nasal skin and underlying structures[3-5] [Figure 1].
Figure 1. Typical implant-related contracted nose deformity. (A) frontal view; (B) lateral view. This figure is quoted with permission from Won et al.[6].
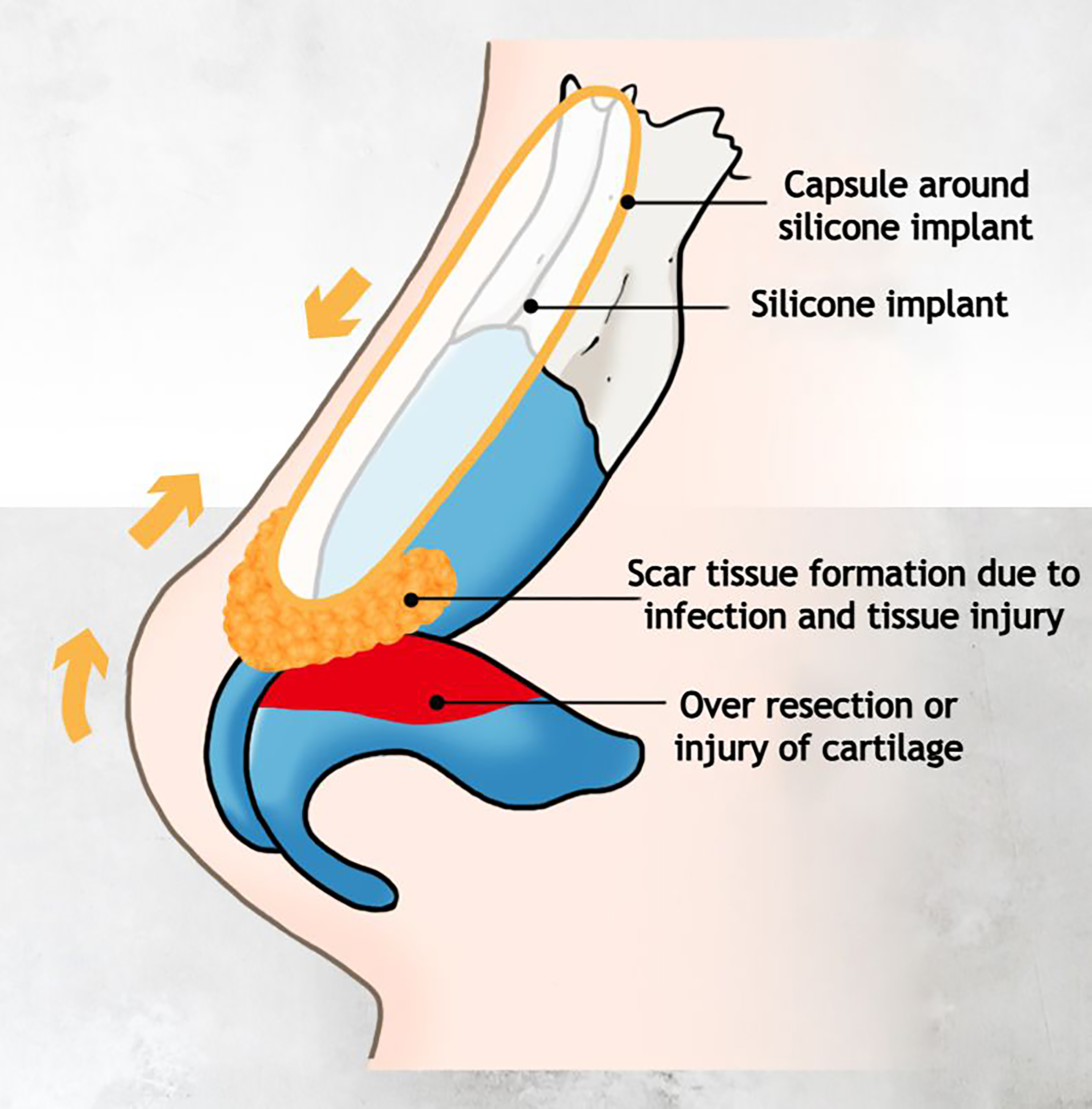
Common causes include over-resection of cartilage with subsequent skin contraction, subacute or chronic capsular contracture related to alloplastic implants, and infection-induced exuberant scar tissue formation[6] [Figure 2].
Figure 2. Typical pathogenesis of contracted nose deformity. This figure is a self-created image, generated using Adobe Illustrator.
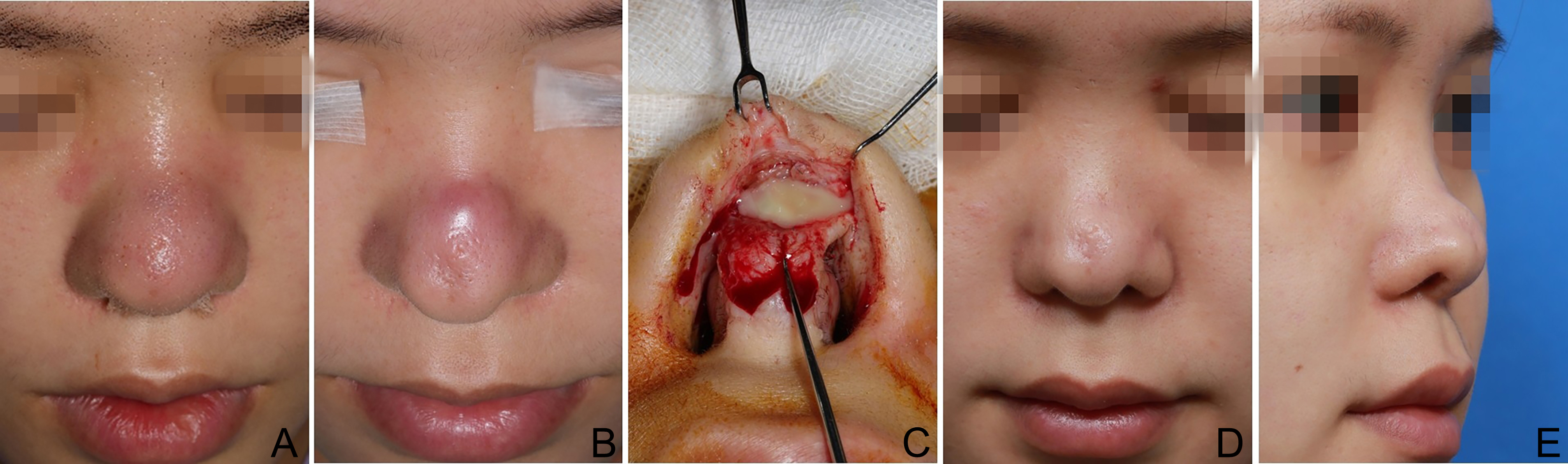
In the Asian contracted nose patient, repeated alloplastic dorsal augmentation is often the cause. Alloplastic implants can induce acute to chronic inflammation, leading to progressive skin envelope damage and pressure-induced necrosis of the lower lateral cartilages (LLCs). Together, they contribute to scar contracture and development of a contracted short nose[1]. When implant infection is present, severe scarring of the skin envelope exacerbates the condition by pulling the already compromised tip cartilages cephalically, resulting in a markedly upturned nasal tip [Figure 3].
Figure 3. Typical development of postoperative contracted nose deformity. (A) Initial presentation with recurrent nasal swelling after rhinoplasty with dorsal silicone implant and rib cartilage tip grafts; (B) Persistent infection despite incision and drainage, irrigation, and antibiotic therapy; (C) Incision and drainage with removal of infected, necrotic rib cartilage grafts via nasal exploration; (D) Frontal view one year after nasal exploration showing residual tip skin dimpling; (E) Right oblique view one year post-exploration demonstrating a low dorsum, cephalic tip rotation, and increased nostril show.
The nasal tip is typically the primary and most severely affected region due to its lack of structural support. As cephalic rotation increases, the nasolabial angle becomes more obtuse, resulting in increased nostril show when viewed from the front[3-5,7]. A deepened nasofrontal angle upon implant removal further accentuates the appearance of nasal shortening. Additional features, such as dorsal skin dimpling and columellar retraction, are also frequently observed. Most postoperative contracted noses exhibit significant structural compromise, including weakened or destroyed alar cartilages and loss of septal support.
Once a contracted nose has developed, its surgical correction becomes highly challenging. One of the primary considerations is determining the optimal timing for revision. In cases involving alloplastic implants complicated by infection, a staged approach is often necessary: prompt removal of the infected implant followed by delayed reconstruction after resolution of inflammation. However, progressive scarring of the overlying soft tissue and necrosis of the underlying cartilage during the healing phase can further complicate secondary reconstruction. The authors have previously reported favorable outcomes with immediate reconstruction using autologous cartilage after implant removal[8], offering potential advantages in reducing tissue contraction while minimizing the risks of infection and graft resorption.
This review presents the natural progression of patient care for the contracted Asian nose - from initial consultation and surgical planning, through operative techniques, to postoperative management - offering comprehensive surgical strategies at each stage.
PATIENT CONSULTATION
A comprehensive understanding of prior surgeries is essential for surgical planning. Details such as the exact number and dates of previous operations, grafting techniques and materials used, and the reasons for revision - including any complications - must be evaluated as thoroughly as possible during history taking.
When operative records are unavailable or incomplete, the importance of a meticulous physical examination becomes even more critical. In such cases, supplementary imaging, particularly computed tomography (CT), can aid in assessing implant migration, graft calcification, or residual deformity. The authors routinely obtain preoperative CT imaging in all cases of contracted nose revision rhinoplasty, as the native anatomy is often significantly altered. Patients should also be counseled that the absence of detailed prior surgical information introduces diagnostic uncertainty, which may affect both intraoperative decision-making and surgical outcomes.
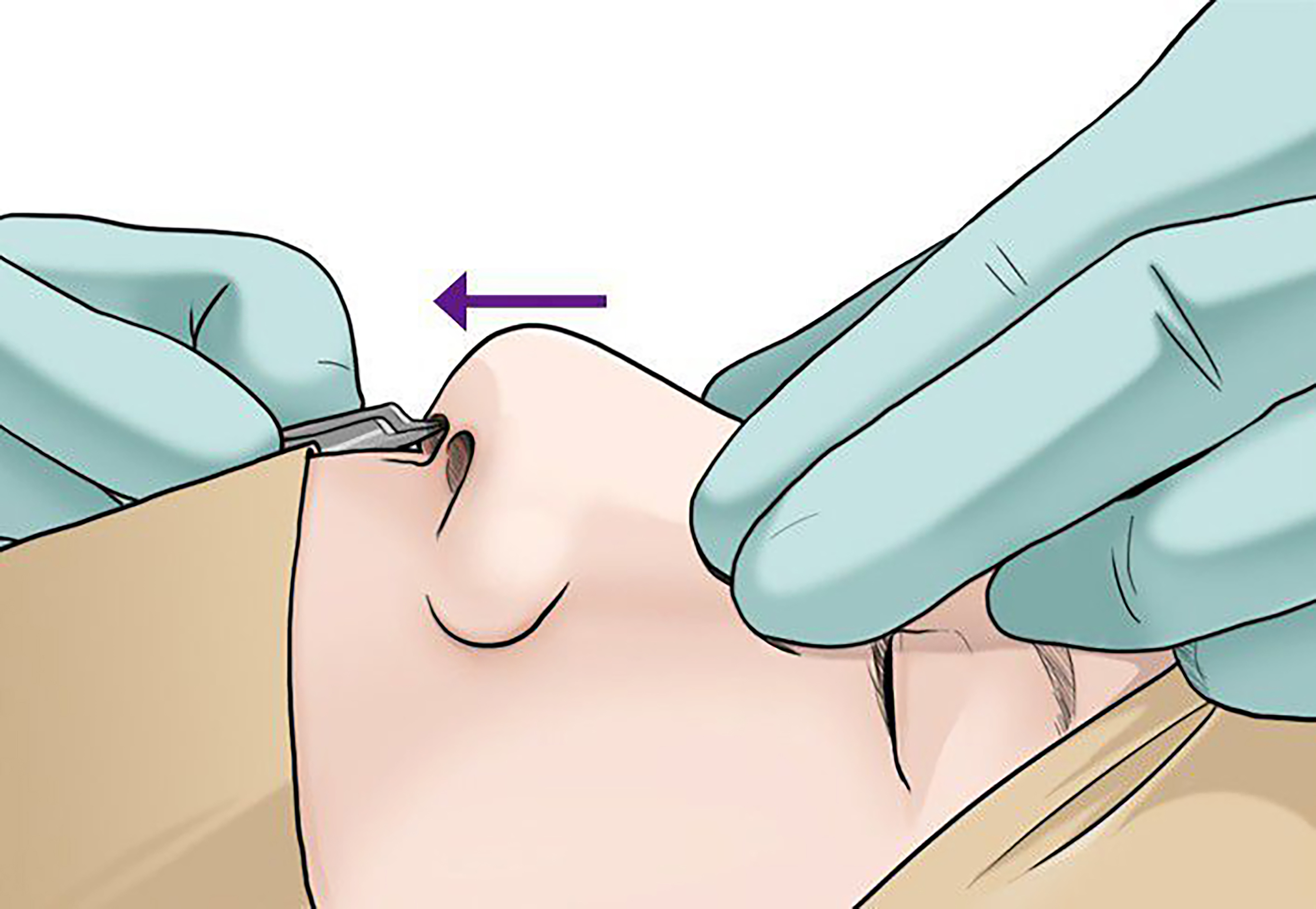
Physical examination should begin with careful palpation of the external nose to assess the skin, underlying bone, and cartilage. Skin mobility can be assessed by applying downward pressure and gentle traction [Figure 4]. Even in cases with a severely upturned tip and tight tip skin, a favorable outcome may still be achievable if the dorsal skin is loose and mobile[9]. If a silicone implant remains on the dorsum and the overlying skin shows some mobility, there is a good chance that the skin will elongate after implant removal. On the other hand, thick, scarred, and immobile skin - especially in cases where the silicone implant has already been removed - may significantly limit the extent of nasal tip lengthening. A contracted skin-soft tissue envelope (SSTE) can make surgical undermining difficult and meticulous care must be taken to avoid further injury.
Figure 4. Intraoperative assessment of skin mobility by pulling the dissected skin and soft tissue envelope over the underlying cartilage framework. This figure is a self-created image, generated using Adobe Illustrator.
The integrity of the nasal septum should be thoroughly evaluated. In many cases, the septal cartilage has already been harvested during previous procedures, and concurrent septal perforations are not uncommon. A seemingly intact septum should be carefully palpated using cotton-tips, as it may reveal a thin, membranous posterior septum with absent cartilage. In severe cases, the caudal septum may also be missing, causing significant tip and columellar contraction [Figure 5]. In such cases, nasal lengthening is possible only after restoring the caudal septum.
Figure 5. A contracted nose with nearly absent columella with severely upturned nasal tip. (A) frontal view; (B) basal view.
Even with extensive structural reconstruction, lengthening the short, contracted nose is challenging, with results often limited to only 3-4 mm of elongation. Therefore, thorough preoperative patient counseling is essential to establish realistic expectations and define achievable surgical goals. In most cases, the objective is not to create an aesthetically ideal nose, but to reestablish a more natural and normalized appearance. The realistic surgical goals include caudal rotation of the tip without severely compromising projection, a smooth and natural dorsal contour, and improvement in skin condition. However, many patients often hold unrealistic expectations, dreaming of a more attractive nose than their original preoperative state.
Successful management of the contracted nose therefore depends on effective patient communication, careful preoperative planning, and surgeon’s experience in managing such complex deformities.
SURGICAL PROCEDURES AND TECHNIQUES
Prior to describing the technical details of each surgical step, it is important to establish a clear understanding of the surgical objectives, core principles, and the variations in strategy based on the severity of nasal contracture.
In mild cases, where tip shortening is minimal and cartilaginous support remains relatively strong, additional cartilage grafting can achieve some degree of caudal tip rotation and dorsal augmentation can create an illusion of nasal lengthening. In moderate to severe cases, a more extensive reinforcement and reconstruction of the nasal framework is necessary to achieve lengthening of the SSTE[9].
Surgical management typically involves three key components:
1. Releasing the contracted SSTE and redraping it.
2. Reconstructing a firm structural framework to support and lengthen the tip.
3. Improving skin quality to minimize the risk of re-contracture.
First, the adherent and contracted SSTE needs to be released[10]. Wide dissection of subcutaneous tissue, scar removal, and horizontal releasing incisions are key techniques. If insufficient, conchal composite grafts bridging mucosal gaps may supplement the deficient vestibular skin and facilitate redraping of the skin.
Next, reconstruction of the framework begins with securing a reliable grafting material. Autologous rib cartilage is often required to replace alloplastic implants due to its superior strength, rigidity, and ample availability. A septal extension graft (SEG) or extended columellar strut, supported by extended spreader grafts (ESGs), provides the structural foundation to reposition the LLCs.
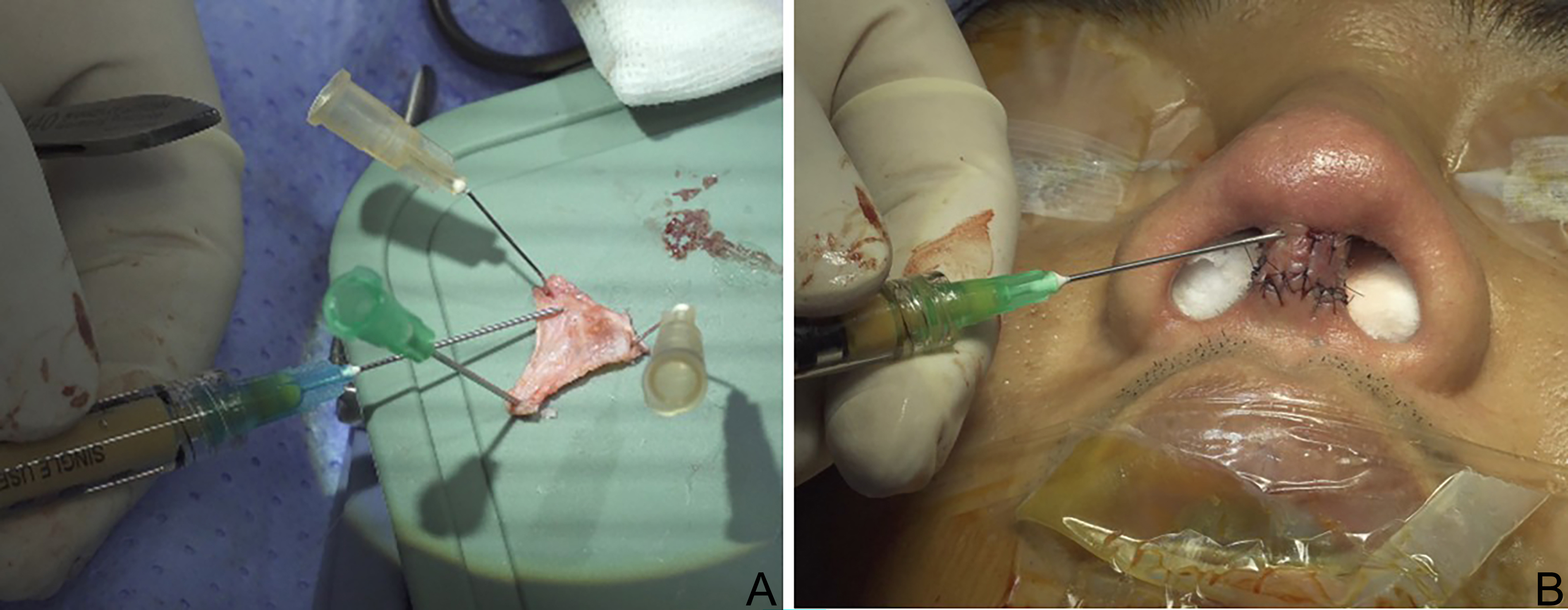
Lastly, improving the skin quality is crucial to prevent re-contracture. It can be enhanced both preoperatively with serial nanofat injections, and intraoperatively through fascia grafting and intradermal nanofat injection to support healing of the damaged skin[11-13] [Figure 6].
Figure 6. Intraoperative fascia grafting and nanofat injection. (A) Nanofat injection into the fascia for tip grafts; (B) Nanofat injection into the columellar wound.
Graft preparation
Successful rhinoplasty begins with careful graft selection and preparation. All grafts should be tailored to the individual patient’s anatomical needs and the specific reconstructive objectives. In patients with contracted noses, septal and conchal cartilage are often depleted due to prior surgeries, typically lacking both volume and rigidity. As a result, although their superiority over other graft materials remains debated[14-16], autologous rib cartilage grafts (RCGs) are preferred in our practice for structural support. Donated costal cartilage can serve as an alternative; however, its resorption rate is generally higher and less predictable compared to autologous RCGs[17]. This unpredictability complicates the design of dorsal augmentation. Also, because thicker segments are required to ensure structural stability despite resorption, there is an increased risk of airway compromise. For this reason, autologous RCGs are commonly adopted for their greater long-term stability and reliability in maintaining structural integrity. The technique for harvesting autologous costal cartilage is well established and has been described in detail in the author’s previous publications[6].
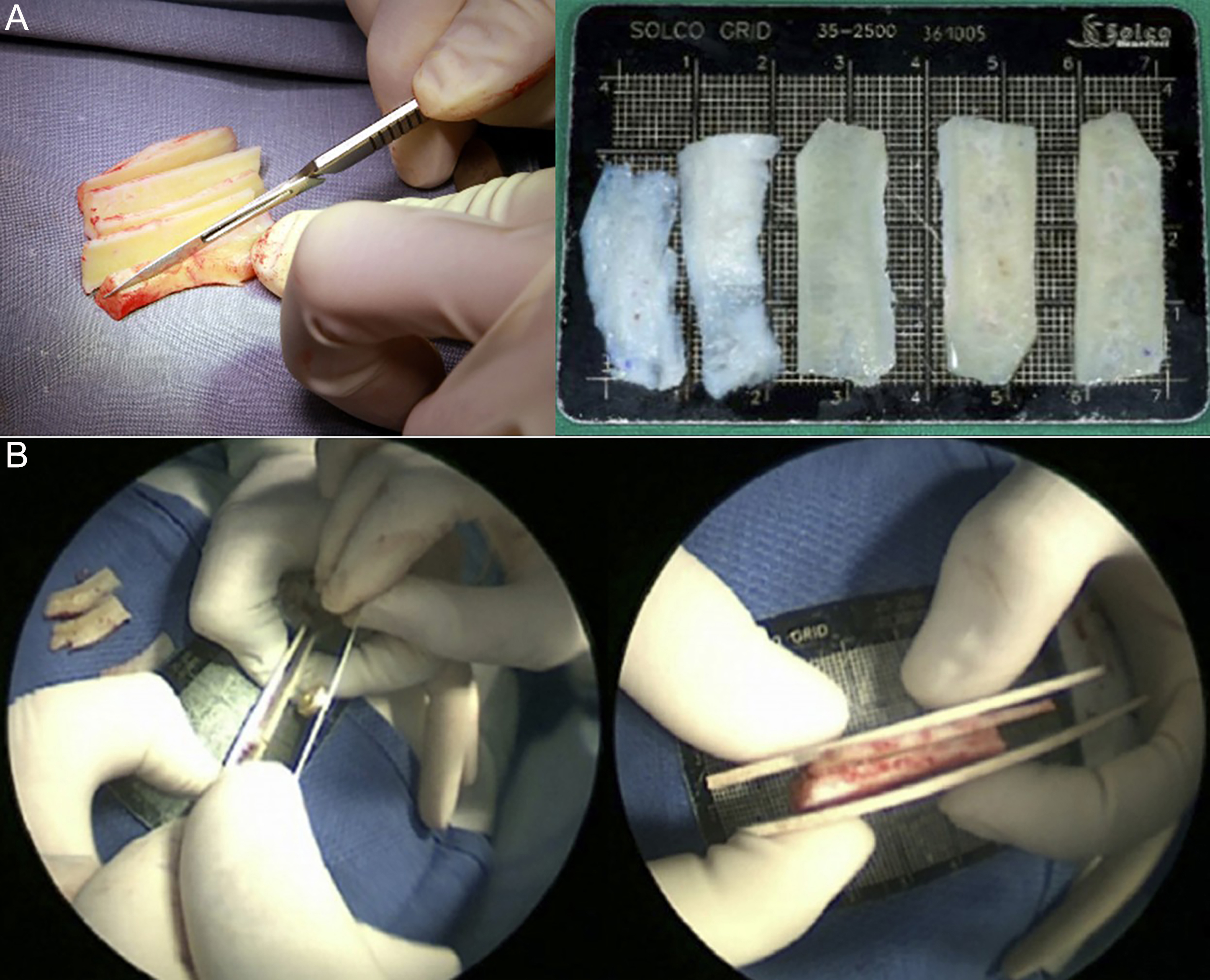
Once harvested, autologous costal cartilage is carved into various shapes depending on the intended grafting purpose while considering the size, shape, and stiffness of the harvested rib. In general, the authors prefer to cut the rib into multiple thin, flat, and straight segments by making longitudinal or tangential cuts [Figure 7A]. These thin segments are versatile, used for various grafting techniques including SEGs, spreader grafts, batten grafts, and even dorsal onlay grafts when stacked in multiple layers [Figure 7B]. This flat, long cartilage slice can resist warping provided that the peripheral portions are kept symmetrical on both sides[18]. If warping does occur, the segments can be split in half and used as bilateral ESGs, effectively compensating for the curvature.
Figure 7. Costal cartilage graft. (A) Carving of costal cartilage into flat, straight slices with symmetrical peripheries to minimize warping; (B) Stacking multiple costal cartilage slices for dorsal augmentation. This figure is quoted with permission from Won et al.[6].
Despite their mechanical advantages, autologous RCGs are not without drawbacks - including potential warping, donor site morbidity, and occasional graft infection. Thus, graft selection should be individualized, balancing the patient’s clinical context with the surgeon’s expertise and experience.
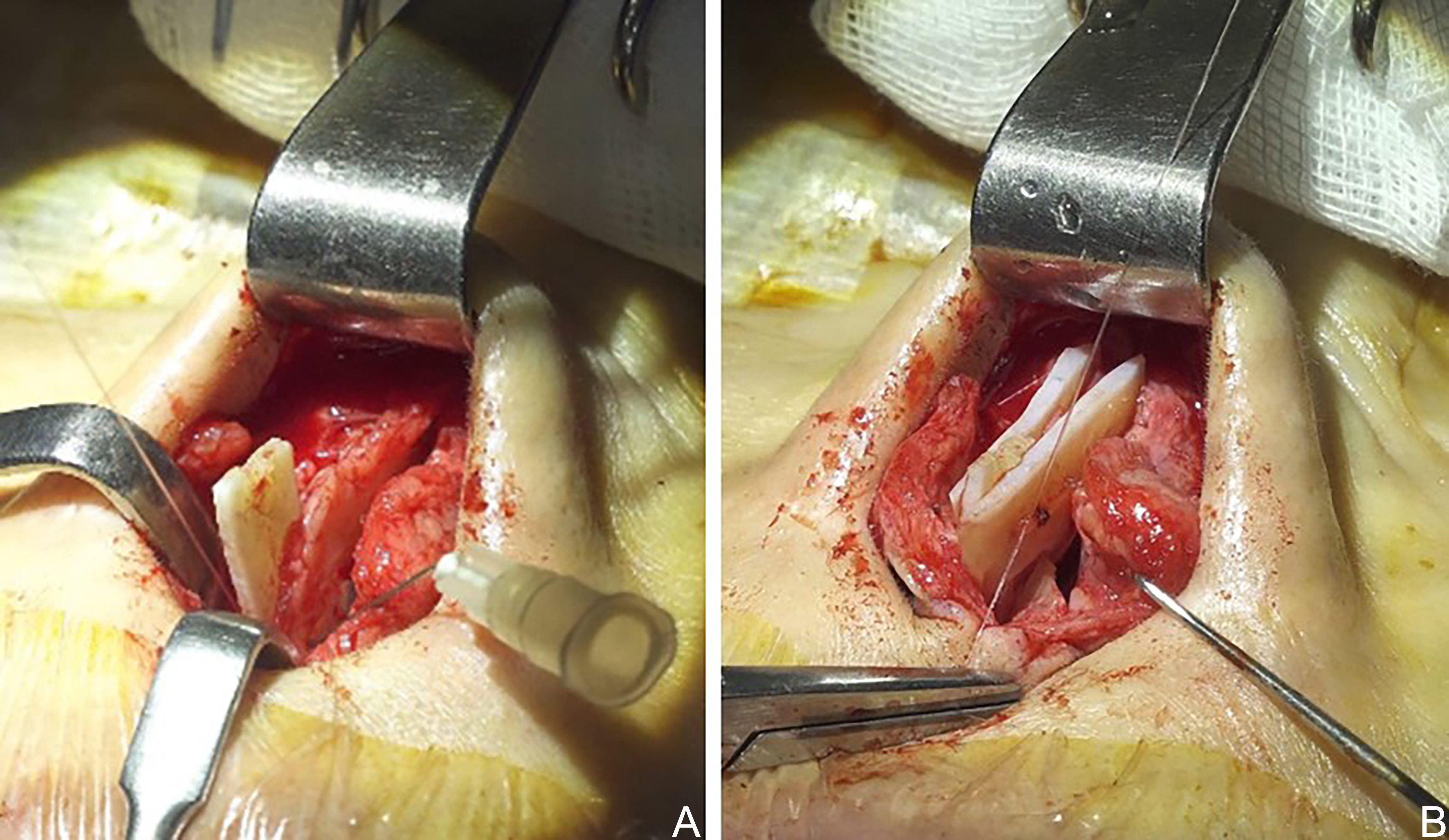
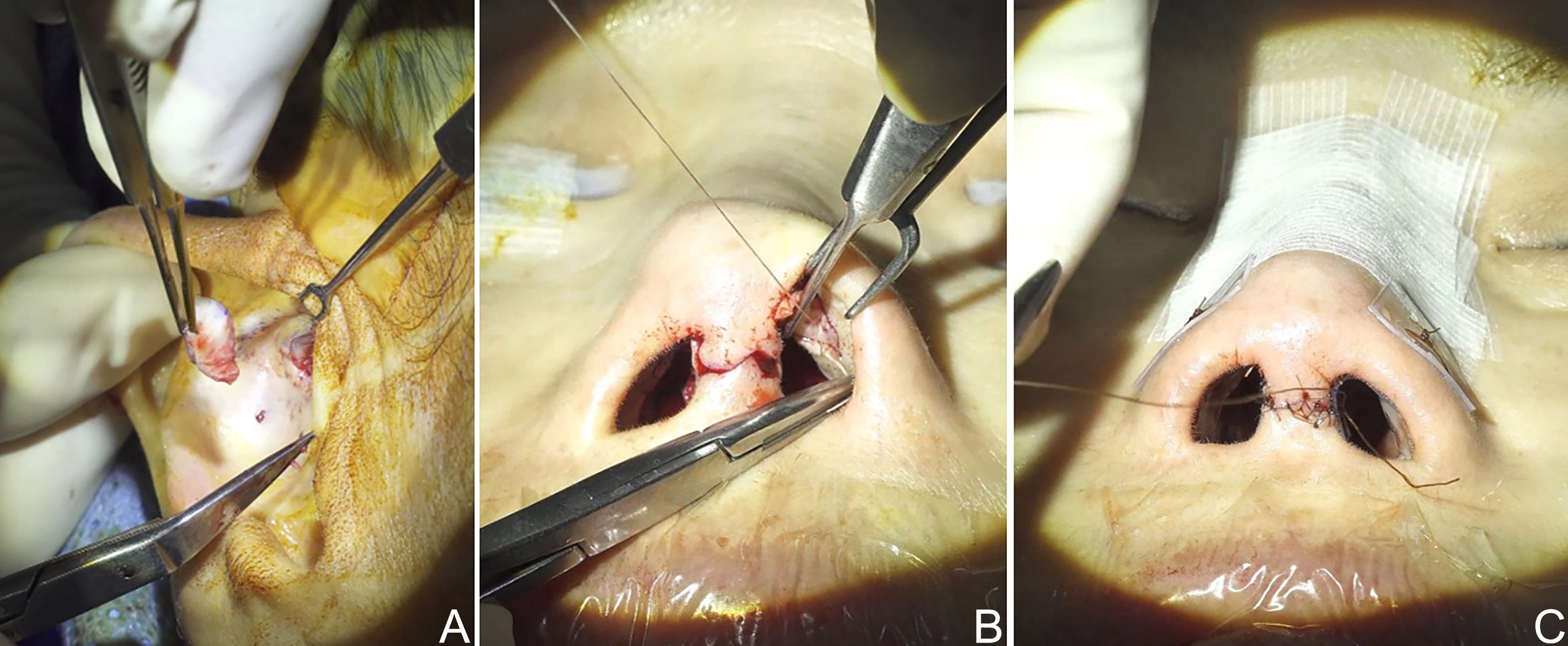
SSTE release
Once graft preparation is complete, the surgical procedure begins with the release of the SSTE. Wide dissection of the SSTE is essential to allow maximum stretching of the skin and proper accommodation of the elongated framework[19,20] [Figure 8A]. Thick scar tissue, particularly over the LLC and at the junction of the lower and upper lateral cartilages (ULCs), should be excised or released to improve skin flexibility and maneuverability. Capsules surrounding silicone implants must be thoroughly removed, as overlying capsules restrict skin stretch, while underlying capsules interfere with proper graft positioning. When scar tissue is excessively thick and adherent to the tip skin, multiple gentle horizontal releasing incisions using a sharp No. 15 blade can further facilitate skin release [Figure 8B].
Framework lengthening
Now that the underlying framework is exposed, reconstruction of the supporting structure begins with repositioning and securing the LLCs. After dividing the LLCs and elevating the septal flap, the septum is first evaluated. In many cases, the caudal septum - and sometimes the entire cartilaginous septum - is deviated, weakened, or even absent. Because the contracted SSTE exerts considerable tension upon redraping, a strong L-strut capable of withstanding this pressure must be reestablished[21]. To stabilize and reinforce the septum, techniques such as re-suturing the posterior septal angle to the anterior nasal spine (ANS), placing a batten graft, or fully replacing the L-strut may be employed.
Once the septum has been stabilized, SEGs reinforced with ESGs are applied. The grafts act as key maneuvers to lengthen the nose and achieve caudal rotation of the nasal tip[7] [Figure 9]. Because thick RCGs on the septum may obstruct the airway, SEGs must be performed in a manner that preserves nasal patency. An end-to-end SEG using a thin, flat piece of cartilage is generally preferred for this reason. However, care must be taken to avoid using a graft that is too weak, as this may result in caudal septal buckling, worsening deviation and nasal obstruction.
Figure 9. Lengthening of the nasal framework. (A) Overlapping SEG; (B) Reinforcement of the SEG with bilateral extended spreader grafts. SEG: Septal extension graft.
Placement of the ESG can be performed either by creating a dorsal mucosal pocket within the septum or by separating the junction between the septum and the ULCs, depending on the anatomical context. Both techniques require attention to avoid airway narrowing caused by excessive thickness of the dorsal or caudal septal components. Beveling and thinning the extended portion of the ESG at its junction with the SEG is essential to prevent excessive bulk in the caudal septum.
Tip repositioning and refinement
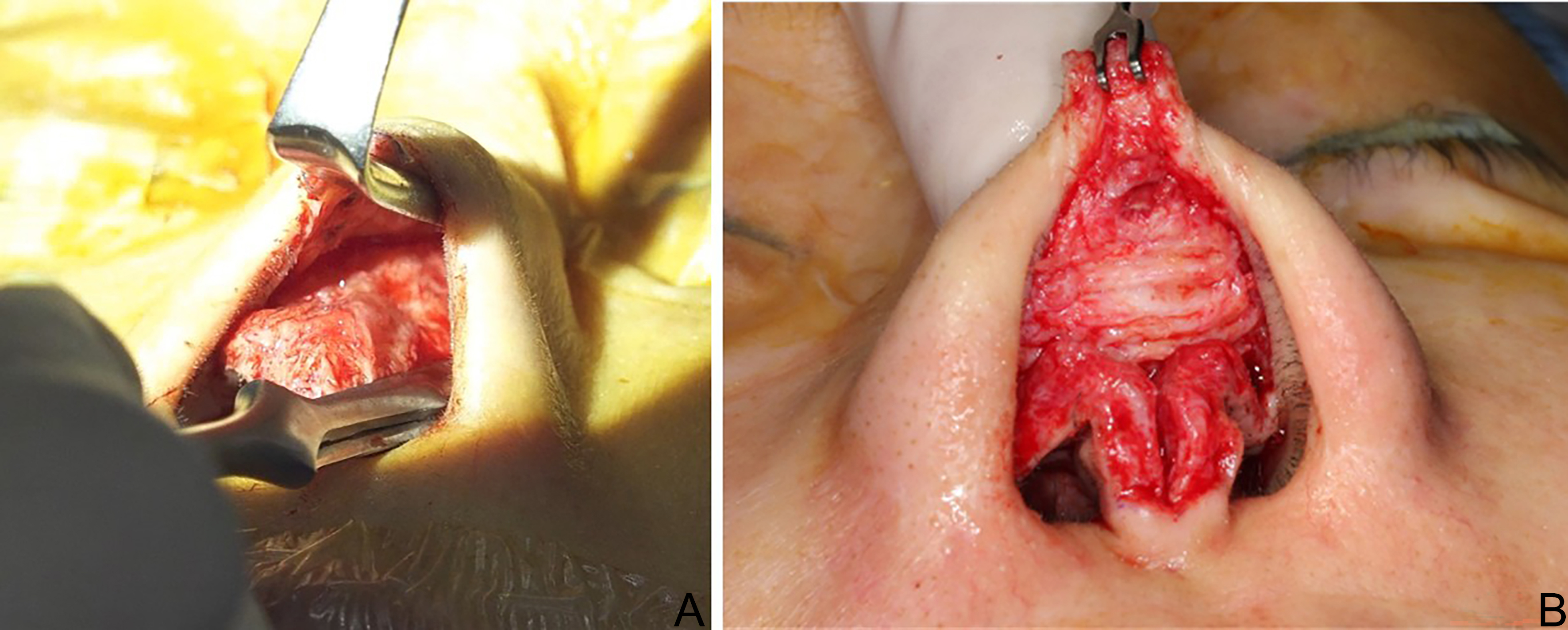
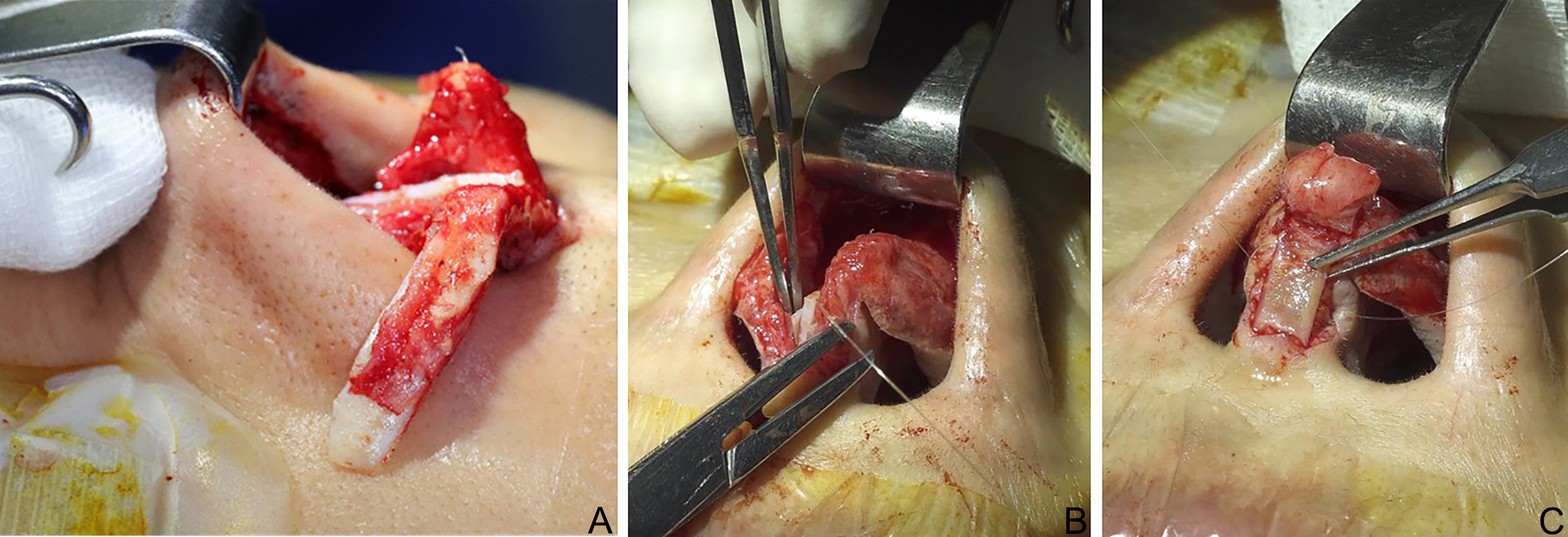
With the structural groundwork in place, the next step is tip refinement. As previously mentioned, the LLCs in contracted noses are often weakened, deficient, and obscured by dense scar tissue[22]. Therefore, after carefully removing the scar tissue, the LLCs should be dissected from the ULCs and the pyriform aperture to allow for proper evaluation of their condition [Figure 10].
Figure 10. Release of the lower lateral cartilage from scar tissue, the upper lateral cartilage, and the pyriform aperture.
If the LLCs appear collapsed or partially destroyed, they can be reinforced with a lateral crural strut or onlay graft after being released from the vestibular mucosa [Figure 11A]. Once reinforced, the LLCs are repositioned onto the SEG, both lowering and de-rotating the nasal tip [Figure 11B]. Additional grafts, such as a shield or cap graft, can be placed on the newly positioned tip to further enhance projection and lengthening[13] [Figure 11C].
Extending the lateral component: lowering the alar rim
While the aforementioned techniques can adequately lengthen the central portion of the nose - namely, the columella and tip lobule - the lateral crura often fail to follow the newly projected central tip. This may result in a pinched tip or retracted alar margins. To achieve a more natural and balanced nostril appearance, additional reinforcement of the lateral structures is often required.
A wing graft [Figure 12A], which extends laterally from the tip graft, can help support the alar margin and prevent pinching when viewed from the front. An alar rim graft is also a useful option for reinforcing the alar margin and can help slightly lower the alar rim. Dissection of the soft tissue along the alar rim should begin at the nasal facet using sharp iris scissors, taking care not to over-widen the pocket. The graft should be designed as a thin, flat piece measuring approximately 2-3 mm in width and 12-15 mm in length. Before insertion, the medial end of the graft should be gently bruised using Brown-Adson forceps. Additionally, repositioning the elongated lateral crural strut complex into a pocket created near the pyriform aperture is another effective technique for supporting the alar margin [Figure 12B].
Figure 12. Techniques to lower the alar rim. (A) Wing graft; (B) Repositioning of the elongated lateral crural strut complex.
Despite these maneuvers, alar rim lowering is limited in the Asian contracted nose patients, due to a stiff, inelastic skin envelope and deficient vestibular skin[9]. In such cases, the authors prefer using a conchal composite graft harvested from the cymba concha to fill the gap between the alar skin and vestibular mucosa, while simultaneously lowering the alar margin. Further details are discussed in the skin management section.
Dorsum management
After completing tip refinement, dorsal contouring should be performed to achieve a harmonious nasal profile. A contracted nose often lacks dorsal volume, making a well-carved, non-warping RCG ideal for dorsal augmentation[7]. After symmetrically trimming the peripheral edges of the costal cartilage, the central core segment is shaped using a No. 10 scalpel into a canoe-like form when viewed from above. When placing the graft, the concave surface should rest against the nasal dorsum, while the dorsal surface presents a gently convex contour when viewed laterally [Figure 13]. To secure the graft onto the bony bridge without migration, any residual silicone capsule should be thoroughly removed, and the graft should be sutured to the ULCs. A strip of costal perichondrium, sutured to the undersurface of the graft at its nasion end, can aid in fixation by anchoring the graft to the bony radix. In such cases, the bony radix should first be roughened with a rasp or minimally dimpled using osteotomes.
Figure 13. Carved costal cartilage with perichondrium placed at the nasion end for dorsal augmentation.
While costal cartilage offers favorable characteristics regarding strength and abundance in volume, it also carries a consistent risk of warping. To reduce this risk, the carved cartilage is periodically soaked in warm saline for 10 min at a time, then removed for further carving. During this repetitive process, the cartilage should be carefully monitored for signs of warping[16]. If warping becomes evident, the remaining concave peripheral portions must be further excised[23,24]. Although the process can be time-consuming, meticulous re-carving of the rib cartilage typically results in a straight, stable graft.
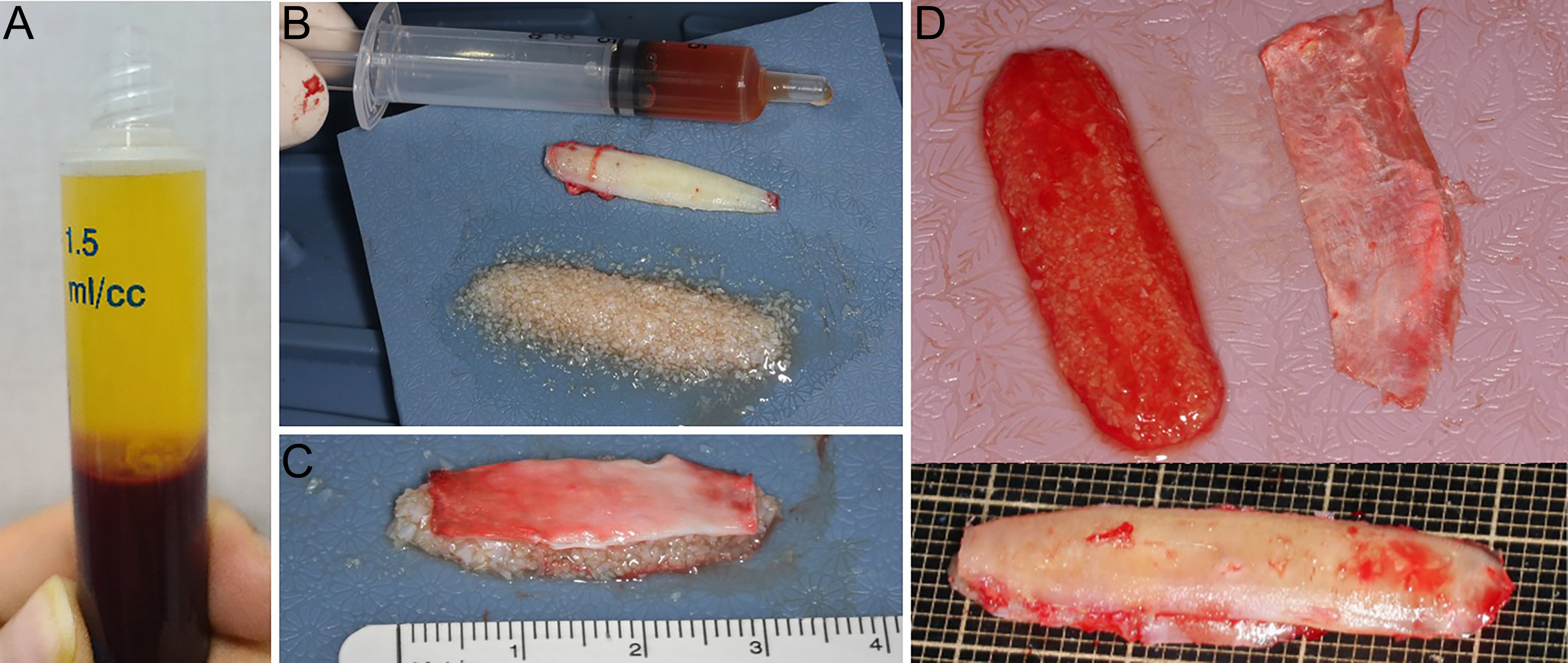
Despite these preventive measures, minor warping may still occur. To address this, the authors frequently employ a two-layer grafting approach for dorsal augmentation: a carved RCG placed underneath, topped with a layer of diced cartilage (DC) mixed with platelet-rich fibrin (DCPRF). The rib cartilage is finely diced using a No. 11 blade into pieces smaller than 1 mm in diameter. Platelet-rich fibrin (PRF) is obtained by centrifuging 10 mL of the patient’s blood at 3,000 rpm for 5 min. The middle PRF layer, along with a portion of the overlying platelet-poor plasma, is aspirated, mixed, and applied to the DC. The resulting fibrin matrix both acts as a scaffold and promotes healing through growth factors released from the platelets[25-28]. After preparation, the DC can be molded into various forms according to the intended grafting purpose [Figure 14]. Although the authors previously used temporalis fascia to wrap DC[29-31], DCPRF has become the preferred alternative. It holds distinct advantages, including reduced invasiveness (eliminating the need for fascia harvest) and improved molding flexibility (easily shaped to match the nasal dorsum)[27,28].
Figure 14. Two-layer grafting technique for dorsal augmentation using diced costal cartilage and PRF. (A) Separation of blood into three layers after centrifugation. The middle PRF layer is collected along with a portion of the upper platelet-poor plasma layer; (B) Diced cartilage, carved cartilage graft, and PRF; (C) Diced cartilage glued with PRF, molded into a dorsal graft, and covered with perichondrium; (D) Two-layer grafting technique: carved rib cartilage, diced cartilage mixed with platelet-rich fibrin, and perichondrium. PRF: Platelet-rich fibrin.
As DCPRF layer placed on top serves to camouflage the underlying carved rib cartilage and mask any minor warping, it is particularly useful in thin-skinned patients, where the shadows of the rib graft are more likely to be visible. Although resorption of DCPRF is minimal, the minor volume gain caused by PRF should be considered to ensure accurate restoration of dorsal contour.
Skin management
Following structural reconstruction, proper repositioning and adaptation of the skin become essential. However, in contracted noses, dimpling or surface irregularity of the nasal skin - particularly around the tip and columella - is common, making skin management a significant challenge. Skin dimpling may result from thinning caused by pressure from a protruding implant, pus drainage in infected cases, or even implant extrusion through the skin [Figure 15]. In more severe cases, extensive dimpling or crumpling of the skin can occur secondary to scar contracture following removal of an infected dorsal implant.
Minor dimpling is best managed with soft tissue and cartilage underlay following skin release. Placement of a cartilage graft topped with perichondrium at the dimpling site is often the preferred technique. In addition, nanofat or platelet-rich plasma (PRP) injections into the dermis may aid in improving skin quality and promoting healing[11-13].
In cases of severe skin contraction, a more complex and delicate approach is required. During dissection, the skin must first be adequately released from the underlying scar tissue. Depressed areas should be augmented with cartilage and soft tissue grafts. Protruding areas require subcutaneous releasing incisions followed by tight taping or bolster cutaneous sutures - often in combination with a silastic sheet to facilitate skin flattening. Hyaluronidase injection into the protruding skin has also been reported as an alternative method for loosening dense scar tissue and preventing fibrosis[32]. Nevertheless, in cases of extensive skin damage, full restoration of normal texture and elasticity is difficult and often requires staged or adjunctive treatments.
Severe contracture or defects of the columella often require composite grafts or local flaps to restore normal anatomical appearance. Particularly in cases where restoration of skin quality is a priority, local flaps are generally preferred[33-35]. However, local flaps carry a potential risk of secondary deformities or visible scarring; thus, their use must be carefully weighed [Figure 16][36].
Figure 16. Reconstruction of a contracted nose with severely damaged skin using a forehead flap; Preoperative and 1-year postoperative view. This figure is quoted with permission from Jin et al.[36].
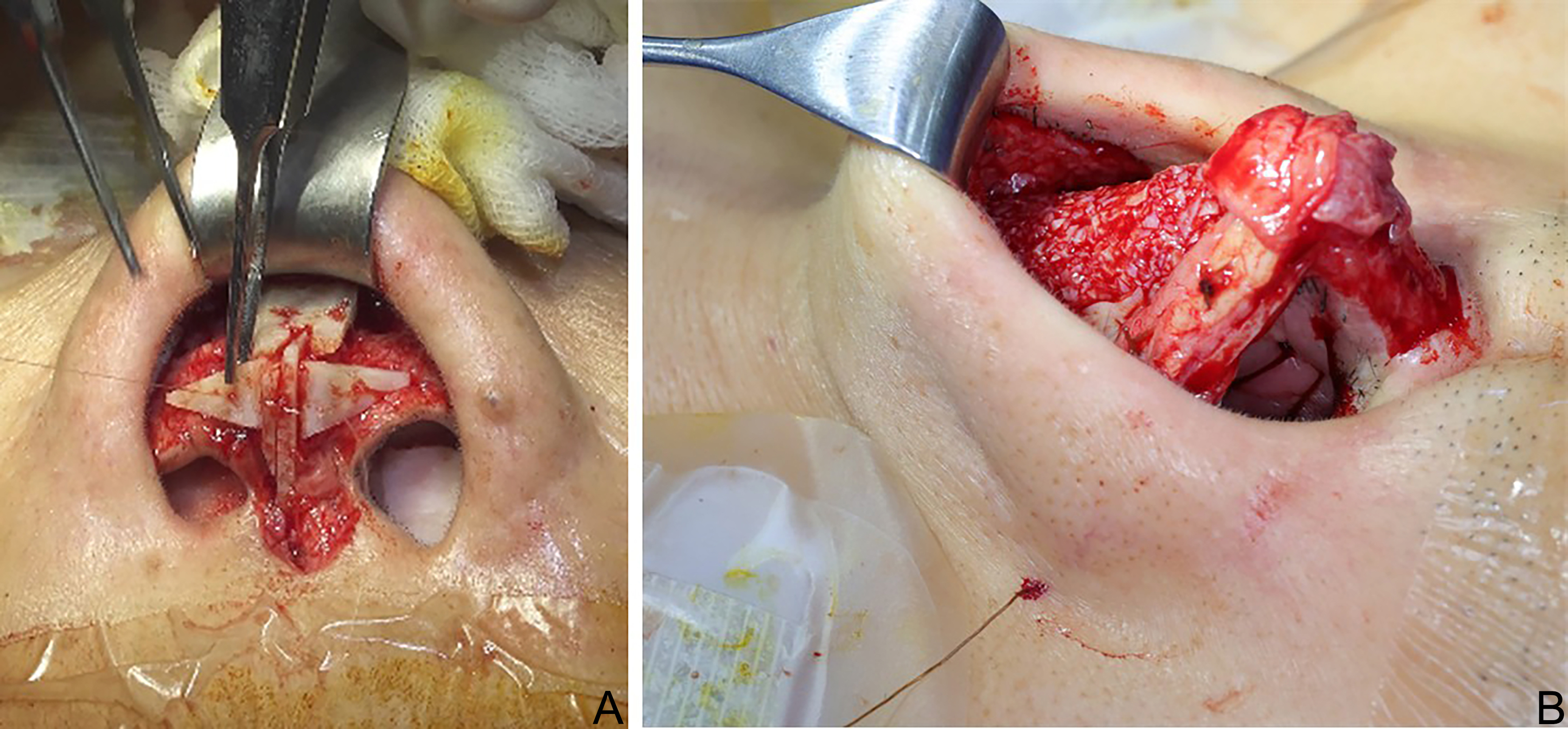
Composite graft
If the contracted skin is insufficient to accommodate the elongated framework and redraping is not feasible, a chondrocutaneous composite graft harvested from the cymba concha is prudently used to fill the gap, particularly in the area of the soft tissue triangle[37] [Figure 17A]. The natural curvature of the cartilage from the cymba concha conforms well to the contour of the graft site. The resulting donor site scar is also typically inconspicuous, making it an ideal graft [Figure 17B].
Figure 17. Conchal composite graft. (A) Conchal cartilage harvested from the cymba concha; (B) Composite graft placed in the soft tissue triangle; (C) Fixation of conchal composite graft using through-and-through sutures with silastic sheet application.
After marking the intended graft shape on the cymba concha, an incision is made through the skin and underlying cartilage while preserving the posterior perichondrium and skin[38]. To enhance graft viability, direct infiltration of anesthetic solution into the harvest site should be avoided[38,39]. Harvest of the graft is completed by dissecting the perichondrium from the posterior surface of the conchal bowl.
If the donor defect is small, primary closure is generally possible. However, if the defect is too large, a full-thickness skin graft (FTSG) - typically harvested from the postauricular area - may be required. In such cases, a slightly larger size than the actual defect is excised to compensate for contraction following graft harvest. Subcutaneous tissue should be removed to enhance skin graft viability. A compression dressing is applied to the cymba concha for 3 to 4 days, and antibiotic ointment is used to keep the wound moist during the initial healing period.
Conchal composite grafting should precede primary closure of the columella. The procedure begins by suturing the caudal end of the graft to the marginal incision line, followed by fixation of the cephalic end to the vestibular incision to fill the defect. Once secured in place, the graft is stabilized with gentle pressure using either internal packing material or through-and-through sutures combined with silastic sheet application[38] [Figure 17C].
SPECIAL CONSIDERATIONS
The importance of skin management in contracted nose deformity cannot be overstated. Even when all surgical principles are meticulously followed, unexpected skin damage may occur, particularly in cases with severe contracture and dense scar tissue. Several adjuvant therapies have recently gained traction for their potential to promote skin and wound healing, contributing to improved outcomes in rhinoplasty.
PRP
In recent years, the use of PRP has gained popularity in rhinoplasty due to its reported efficacy in enhancing skin healing[40]. PRP contains growth factors such as vascular endothelial growth factor (VEGF) and platelet-derived growth factor (PDGF), which promote cell proliferation and collagen synthesis, thereby facilitating wound healing[40]. When applied in combination with fat grafts, PRP has been shown to yield superior outcomes in preventing skin necrosis by further promoting angiogenesis and tissue regeneration[11,40-42]. While PRP presents a promising option for patients with compromised skin, its use should be tailored to individual patient needs and guided by the surgeon’s clinical experience, as a universal protocol has yet to be established.
Hyperbaric oxygen therapy
Hyperbaric oxygen therapy (HBOT) has also gained increasing attention in recent years as an adjuvant modality to support recovery after rhinoplasty[43,44]. The therapy involves inhaling 100% oxygen within a pressurized chamber, which enhances tissue repair and regeneration by increasing the amount of oxygen dissolved in plasma. Improved oxygen delivery to peripheral tissues stimulates angiogenesis and collagen synthesis, while also enhancing immune function, which helps prevent postoperative infections. Clinical studies have demonstrated its benefit in ischemic soft tissue wounds and compromised nasal skin following rhinoplasty[43-45].
Although no universally accepted protocol exists, HBOT for postoperative healing is typically administered at pressures ranging from 1.5 to 3.0 atmospheres absolute (ATA), with each session lasting 45 to 120 min[46]. For rhinoplasty patients, 10 to 20 dives are generally recommended, but the total number may vary depending on the extent and severity of skin damage and the individual’s healing response. Early initiation of HBOT is generally advised to maximize therapeutic benefit.
LIMITATIONS
Numerous techniques have been outlined in the literature for revision rhinoplasty in patients with severe nasal contracture. Authors such as Rosenberger et al. and Gunter et al. have emphasized structural grafting, septal reconstruction, and soft tissue redraping as core principles in revision rhinoplasty[47,48]. While our approach is grounded in these core surgical principles, it is further tailored to the unique anatomical characteristics commonly observed in Asian patients.
Table 1 summarizes the challenges, complications, and preferred management strategies and their limitations based on the authors’ clinical experience.
Challenges, management strategies, and limitations in contracted Asian nose revision rhinoplasty
| Challenges/Complications | Management strategies | Limitations/Precautions |
| Adherent, contracted SSTE | Wide dissection of subcutaneous tissue Scar removal ± Horizontal releasing incisions Alloplastic capsule removal | |
| Deviated, weakened septum | Re-suturing the PSA to the ANS Batten graft | |
| Depleted septal, conchal cartilage | Rib cartilage graft | Donor site morbidity (e.g., pneumothorax) Warping |
| Short nose with upturned tip | Septal extension graft + Extended spreader graft Shield graft or cap graft | Airway obstruction due to thickened septum Caudal septal buckling |
| Collapsed, destroyed LLC | Lateral crural strut or onlay graft | |
| Retracted alar margin | Wing graft or alar rim graft Lateral crural strut complex repositioning | Deficient vestibular skin |
| Lack of dorsal volume | Carved costal cartilage dorsal onlay graft DCPRF | Warping Volume loss due to resorption |
| Skin dimpling, necrosis | Soft tissue and cartilage underlay Nanofat or PRP dermal injection HBOT | |
| Severe skin contracture, defect | Local flap (e.g., forehead flap) Conchal composite graft | Secondary deformity Donor site scarring |
While we have outlined a range of techniques tailored to various clinical scenarios, revision rhinoplasty for contracted noses often presents unpredictable intraoperative findings that require flexibility in decision-making. Given the heterogeneity of patient presentations, a single standardized approach may not be universally applicable. Furthermore, the use of emerging adjuncts such as PRP and HBOT must be approached with caution, as long-term clinical data supporting their efficacy remain limited. Their application should be guided by careful patient selection and clinical judgment.
CASE PRESENTATION
The following are two representative cases of contracted nose deformity, illustrating the clinical application of the techniques described above.
Case 1
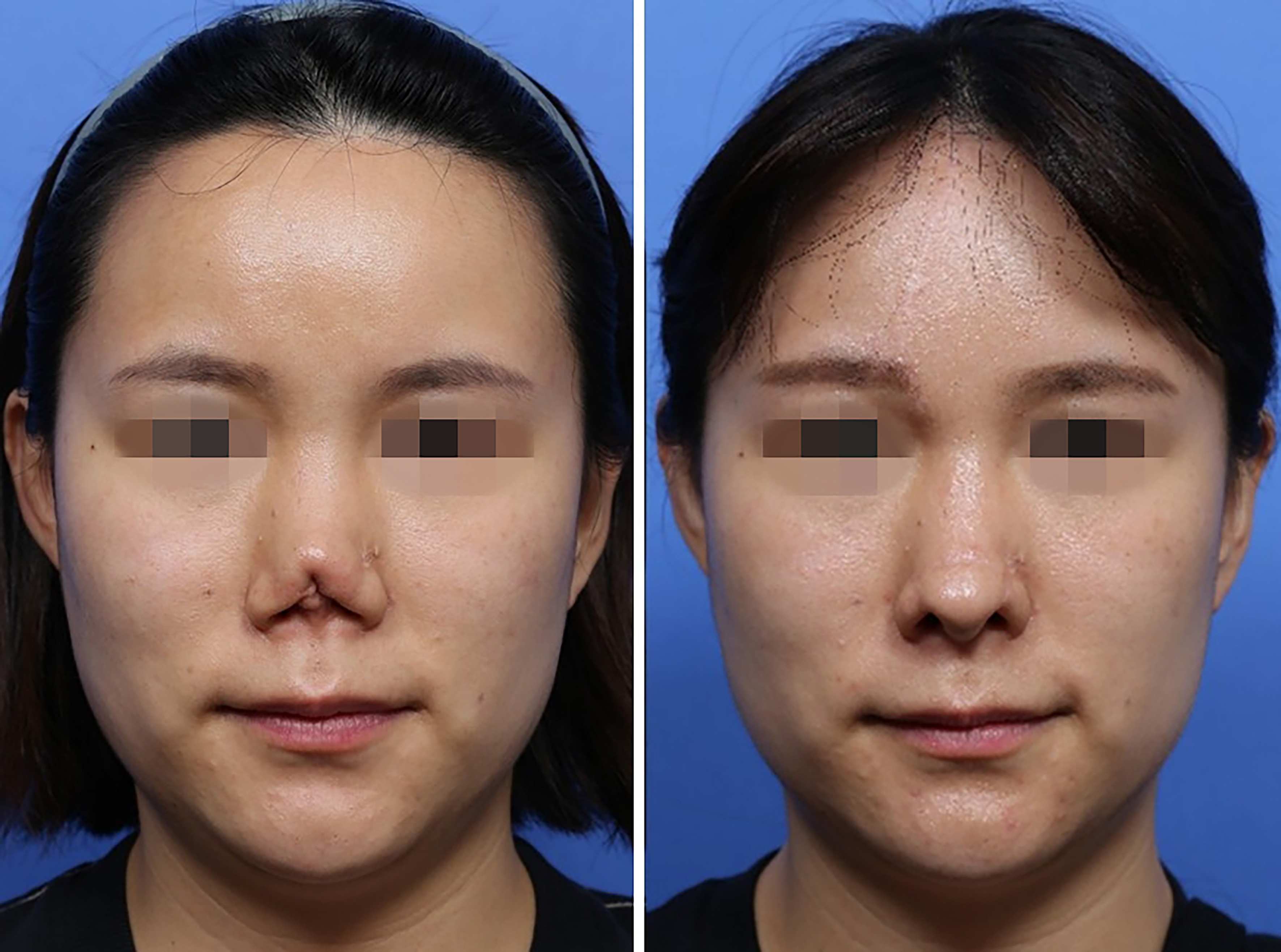
A 69-year-old woman presented for revision rhinoplasty due to dissatisfaction with the shape of her nose. She had previously undergone two rhinoplasties using silicone implants. After the second surgery, her nose gradually developed signs of contraction with an upturned tip and retracted columella.
Revision rhinoplasty involved removal of a 5 mm thick silicone implant and excision of exuberant scar tissue near the tip cartilage and supratip area. Wide skin-soft tissue undermining was performed to mobilize the contracted envelope. Structural reconstruction included framework lengthening with a SEG, bilateral ESGs using autologous rib cartilage, and tip refinement with an onlay graft and infratip lobular graft. Dorsal augmentation was performed using rib cartilage combined with chest soft tissue. A conchal composite graft was also placed inside the nasal vestibule to address skin defect [Figure 18].
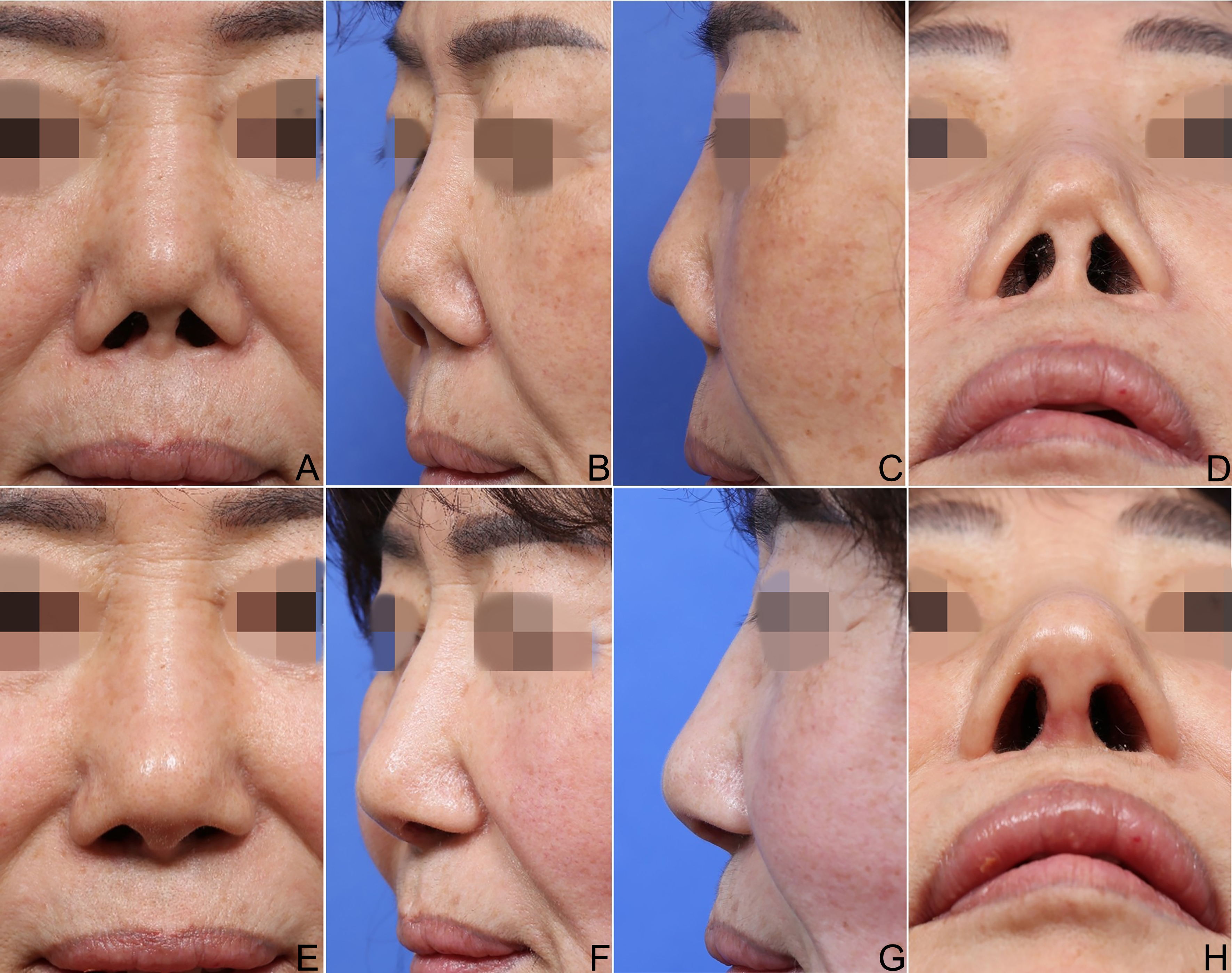
Case 2
A 50-year-old woman sought for revision rhinoplasty for a severely contracted nose. She had a history of eight prior rhinoplasties, the most recent of which was performed three years ago and involved an infected silicone implant. She presented with classic contracted nose deformity after silicone implant removal; a short, upturned nasal tip with severe nostril show, a significantly depressed dorsum, and tip skin dimpling
Revision surgery involved wide skin-soft tissue undermining, excision of scar tissue, and structural reconstruction using an overlapping SEG. The previously displaced tip cartilage was released, repositioned, and topped with cap grafts to lengthen the tip. Dorsal augmentation was performed using a combination of carved rib cartilage and DCPRF to restore volume and smooth the nasal contour. One-year postoperative views [Figure 19E-H] demonstrate marked improvement in both shape and overlying skin quality.
CONCLUSION
Contracted nose deformity is a challenging complication, particularly common among Asian patients with a history of alloplastic implantation. Correction requires more than simply restoring structure - it demands a comprehensive surgical strategy that addresses both the underlying framework and the overlying SSTE.
Successful reconstruction begins with thorough patient counseling to establish realistic expectations and meticulous presurgical planning. Regarding surgical techniques, release of contracted soft tissues, robust framework rebuilding with autologous rib cartilage, and careful redraping of the skin. Special attention must also be given to improving skin quality and managing surface irregularities to minimize the risk of recurrence.
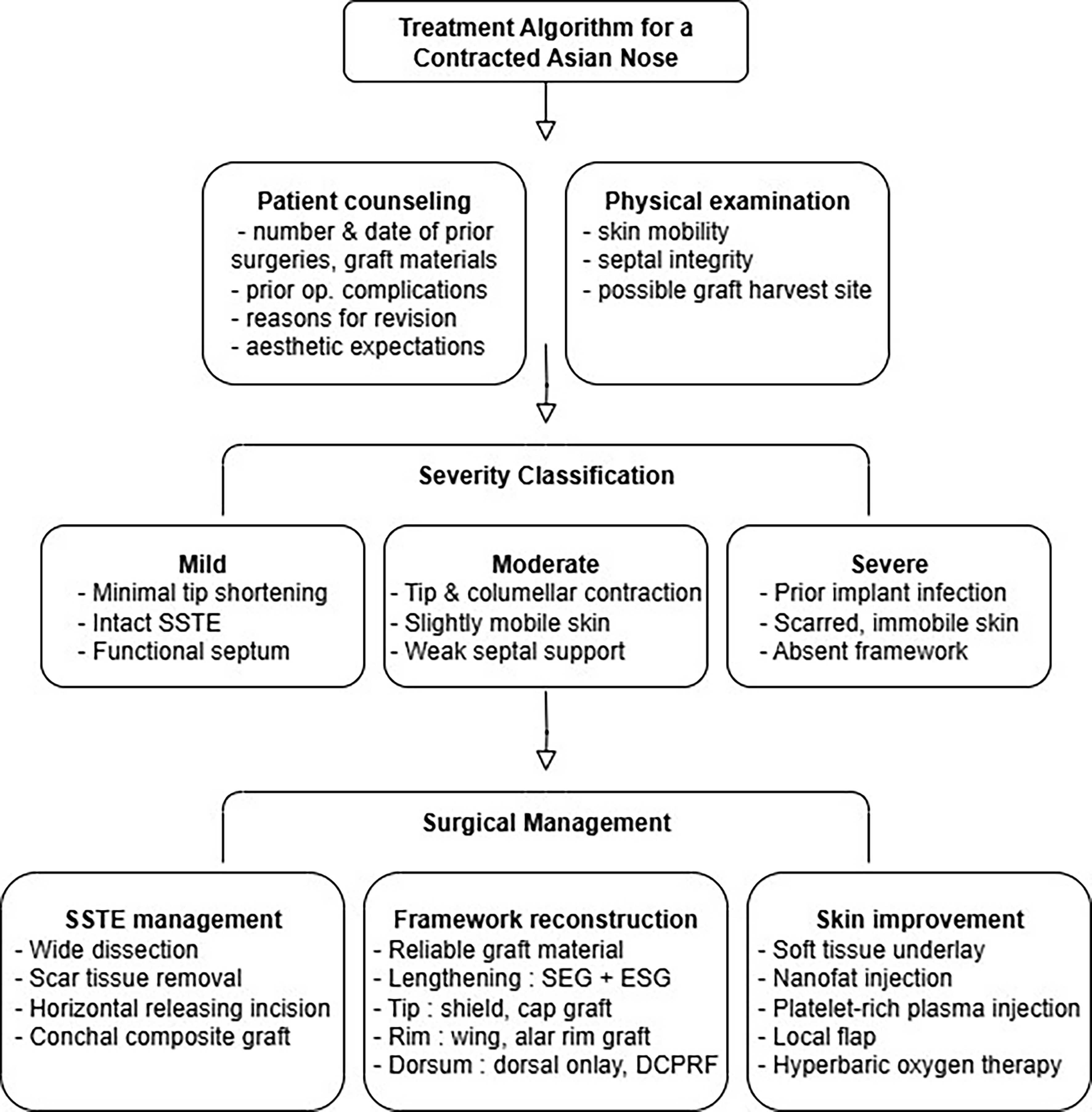
To support practical clinical decision-making, Figure 20 illustrates a treatment algorithm summarizing our approach to assessment, classification, and surgical planning in contracted Asian nose deformity.
A surgeon’s expertise, combined with a thoughtful, individualized approach, is critical to optimizing outcomes in these complex revision cases.
DECLARATIONS
Authors’ contributions
Made conception and design of the study: Jin HR, Won TB
Performed data analysis and interpretation: Jin S
Performed data acquisition and provided resources including figures: Jin HR
Wrote the first draft of the manuscript: Jin S
Contributed to revision and editing of the manuscript: Jin HR, Won TB
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Patient informed consent has been obtained and submitted as supplementary documents.
Consent for publication
Written informed consent for publication was obtained from patients included in this study.
Copyright
© The Author(s) 2025.
REFERENCES
2. Lan MY, Jang YJ. Revision rhinoplasty for short noses in the Asian population. JAMA Facial Plast Surg. 2015;17:325-32.
3. Kim YK, Shin S, Kang NH, Kim JH. Contracted nose after silicone implantation: a new classification system and treatment algorithm. Arch Plast Surg. 2017;44:59-64.
4. Hong DW, Oh JH, Wang J, Kim TH, Kim YC, Choi JW. A grading system-guided approach to the severely contracted nose. Aesthetic Plast Surg. 2024;48:3596-603.
5. Wang X, Zeng W, Sun Y, et al. New classification system of contracted nose and its treatment algorithm. J Plast Reconstr Aesthet Surg. 2023;85:414-22.
6. Won T, Jin H. Revision rhinoplasty using autologous rib cartilage in Asians. Plast Aesthet Res. 2019;6:6.
7. Park JH, Mangoba DC, Mun SJ, Kim DW, Jin HR. Lengthening the short nose in Asians: key maneuvers and surgical results. JAMA Facial Plast Surg. 2013;15:439-47.
8. Won TB, Jin HR. Immediate reconstruction with autologous cartilage after removal of infected alloplast in revision rhinoplasty. Otolaryngol Head Neck Surg. 2012;147:1054-9.
9. Li J, Liang X, Yu L, et al. Short nose lengthening in primary and revision rhinoplasty in Asians. J Craniofac Surg. 2023;34:480-4.
10. Naficy S, Baker SR. Lengthening the short nose. Arch Otolaryngol Head Neck Surg. 1998;124:809-13.
11. Oh YH, Seo JW, Oh SJ, et al. Correction of severely contracted nose. Plast Reconstr Surg. 2016;138:571-82.
12. Kovacevic M, Kosins AM, Göksel A, Riedel F, Bran G, Veit JA. Optimization of the soft tissue envelope of the nose in rhinoplasty utilizing fat transfer combined with platelet-rich fibrin. Facial Plast Surg. 2021;37:590-8.
13. An Y, Wang G, Shang Y, et al. Autologous shuffling lipo-aspirated fat combined mechanical stretch in revision rhinoplasty for severe contractures in Asian patients. Aesthetic Plast Surg. 2023;47:282-91.
15. An Y, Zhao J, Lu L, Zhen Y, Tan X, Li D. Use of autologous costal cartilage combined with expanded polytetrafluoroethylene in Asian rhinoplasty. Chinese Journal of Plastic and Reconstructive Surgery. 2020;2:69-77.
18. Adams WP Jr, Rohrich RJ, Gunter JP, Clark CP, Robinson JB Jr. The rate of warping in irradiated and nonirradiated homograft rib cartilage: a controlled comparison and clinical implications. Plast Reconstr Surg. 1999;103:265-70.
19. Patel PN, Longino E, Most SP. The excessively short nose: our systematic approach. Plast Aesthet Res. 2024;11:20.
20. Tan X, Sun H, Yao P, et al. Application of external nasal skin stretching in Asian rhinoplasty. Ann Plast Surg. 2023;90:S139-42.
21. Peng GL, Azizzadeh B. Correction of the overly shortened nose. Oral Maxillofac Surg Clin North Am. 2021;33:125-9.
22. Jung DH, Moon HJ, Choi SH, Lam SM. Secondary rhinoplasty of the Asian nose: correction of the contracted nose. Aesthetic Plast Surg. 2004;28:1-7.
23. Toriumi DM, Becker DG. Harvesting of autogenous tissue. In: Toriumi DM, Editor. Rhinoplasty dissection manual. Philadelphia: Lippincott Williams & Wilkins; 1999. pp. 139-42.
24. Kim DW, Shah AR, Toriumi DM. Concentric and eccentric carved costal cartilage: a comparison of warping. Arch Facial Plast Surg. 2006;8:42-6.
25. Dohan DM, Choukroun J, Diss A, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e37-44.
26. Rabie AN, El Samny TA, Askoura AM, Desouky MS, Aty AMKA. The functional and aesthetic results of fibrin glue, platelet-rich plasma (PRP), and warm blood as a scaffold for diced cartilage in saddle nose deformity: a descriptive study. Facial Plast Surg. 2025;Epub ahead of print.
27. M Alharbi S, H Alotaibi G, A Alshehri A, J Asiry A, S Alahmari M. Efficacy and safety of platelet-rich fibrin combined with diced cartilage in rhinoplasty: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2025;282:2887-97.
28. Kulaksiz Y, Yenigün A, Şerif Aydin M, Doğan R, Tuğrul S, Özturan O. Effects of platelet-rich plasma and concentrated growth factor on viability of ultra-diced cartilage grafts in a rabbit model. J Oral Maxillofac Surg. 2024;82:1067-75.
29. Park P, Jin HR. Diced cartilage in fascia for major nasal dorsal augmentation in Asians: a review of 15 consecutive cases. Aesthetic Plast Surg. 2016;40:832-9.
30. Daniel RK, Calvert JW. Diced cartilage grafts in rhinoplasty surgery. Plast Reconstr Surg. 2004;113:2156-71.
32. Nele G, Tambasco D, Cavaliere A. Hyaluronidase: a new and powerful ally for post-rhinoplasty fibrosis. Aesthetic Plast Surg. 2025;49:1626-7.
33. Graf AE, Kaplowitz L, Butts SC. Nasal lining reconstruction with loco-regional flaps. Facial Plast Surg Clin North Am. 2024;32:229-37.
34. Jin HR, Jeong WJ. Reconstruction of nasal cutaneous defects in Asians. Auris Nasus Larynx. 2009;36:560-6.
35. Han DH, Mangoba DC, Lee DY, Jin HR. Reconstruction of nasal alar defects in asian patients. Arch Facial Plast Surg. 2012;14:312-7.
36. Jin HR, Kim SJ. An infected absorbable plate: a rare source of persistent tip infection and deformity. Korean J Otorhinolaryngol-Head Neck Surg. 2025;Epub ahead of print.
37. Kim YC, Choi JW. Use of auricular composite graft in rib cartilage-based rhinoplasty for contracted nose correction. Plast Reconstr Surg. 2025;155:492e-501.
38. Yamasaki A, Dermody SM, Moyer JS. Reducing risks of graft failure for composite skin-cartilage grafts. Facial Plast Surg Clin North Am. 2023;31:289-96.
39. Sazgar AA, Sazgar AK, Hatami N, Sazgar MA. Single-stage alar nostril ring correction using auricular composite grafts in reconstructive rhinoplasty. Aesthet Surg J. 2025;45:255-63.
40. Gode S, Ozturk A, Kısmalı E, Berber V, Turhal G. The effect of platelet-rich fibrin on nasal skin thickness in rhinoplasty. Facial Plast Surg. 2019;35:400-3.
41. Beaudoin PL, Carles G. Platelet-rich fibrin in rhinoplasty: a precise and standardized approach. Eur Ann Otorhinolaryngol Head Neck Dis. 2023;140:317-21.
42. Fakih-Gomez N, Manay R, Nazari S, Martins L, Muñoz-Gonzalez C. Regenerative nanofat membrane development process. Aesthetic Plast Surg. 2025;49:3207-23.
43. Kerolus JL, Nassif PS. Treatment protocol for compromised nasal skin. Facial Plast Surg Clin North Am. 2019;27:505-11.
44. Simman R, Bach K. Role of hyperbaric oxygen therapy in cosmetic and reconstructive surgery in ischemic soft tissue wounds: a case series. Eplasty. 2022;22:e61.
45. Tambasco D, Albanese R, Tomaselli F, Montes C. The present and future role of hyperbaric oxygen therapy in plastic surgery. Aesthetic Plast Surg. 2025;49:1583-4.
46. Mortada H, González JE, Husseiny YM, et al. Efficacy of hyperbaric oxygen therapy as an adjunct in aesthetic surgery: a systematic review and meta-analysis of postoperative outcomes and complications. Aesth Plast Surg. 2025;49:2498-512.
47. Gunter JP, Rohrich RJ. Lengthening the aesthetically short nose. Plast Reconstr Surg. 1989;83:793-800.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Special Topic
Copyright
Data & Comments
Data






















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at [email protected].