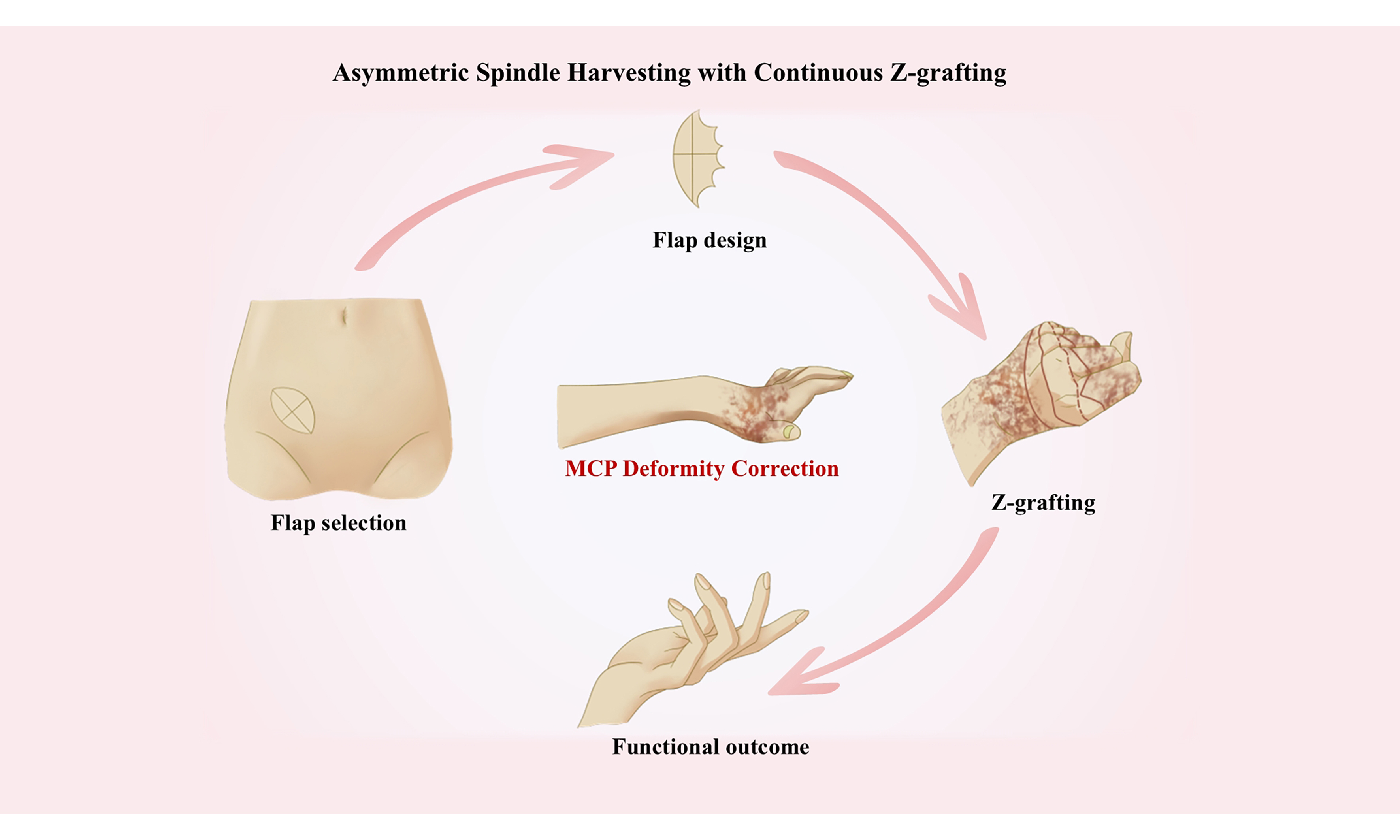
Asymmetric spindle skin harvesting combined with continuous Z skin grafting: experience in correcting metacarpophalangeal joint dorsiflexion deformities
Abstract
Dorsiflexion deformity of the metacarpophalangeal (MCP) joint is a common complication of hand burns, often leading to severely compromised hand function and aesthetics. Traditional surgical techniques typically involve extensive skin harvesting and grafting with splicing, which may increase procedural risks and donor site morbidity, as well as complications such as graft failure, infection, and necrosis. These limitations highlight the need for a surgical approach that can effectively correct scar contracture deformities while minimizing operative challenges and risks, improving graft survival, and promoting functional recovery. Based on the clinical surgical outcomes of 12 patients, we propose a novel technique involving asymmetric spindle-shaped excision combined with continuous Z skin grafting. This approach aims to optimize therapeutic outcomes through personalized scar excision and contracture release, utilizing asymmetric fusiform skin removal, an ultra-tension-reducing suture technique, continuous Z skin grafting, and functional fixation. This article outlines the surgical procedure, technical points, and clinical effects of the proposed method. Ultimately, this method effectively corrects MCP joint dorsiflexion deformities in burn patients, significantly improving both hand function and appearance.
Keywords
INTRODUCTION
Burn injury poses a major health challenge on a global scale, resulting in approximately 11 million individuals seeking medical intervention annually, 30%-40% of whom sustain hand injuries[1-4]. It is highly vulnerable to post-burn complications given the intricate structure and functional complexity of the hands, particularly scar contracture-induced metacarpophalangeal (MCP) joint dorsiflexion deformities[5-7]. Generally, the proposed deformities stem from the anatomical characteristics of dorsal hands, namely thin skin and minimal subcutaneous fat, which predispose them to extensive scarring after burns. Moreover, finger extension and grip function may be seriously impaired owing to MCP hyperextension, interdigital web contractures, and wrist flexion resulting from damaged extensor tendons and joint capsules due to deep burns[8-10]. Critically, progressive contractures, if left untreated, may shorten neurovascular bundles and tendons, ultimately exacerbating functional deficits[11-14].
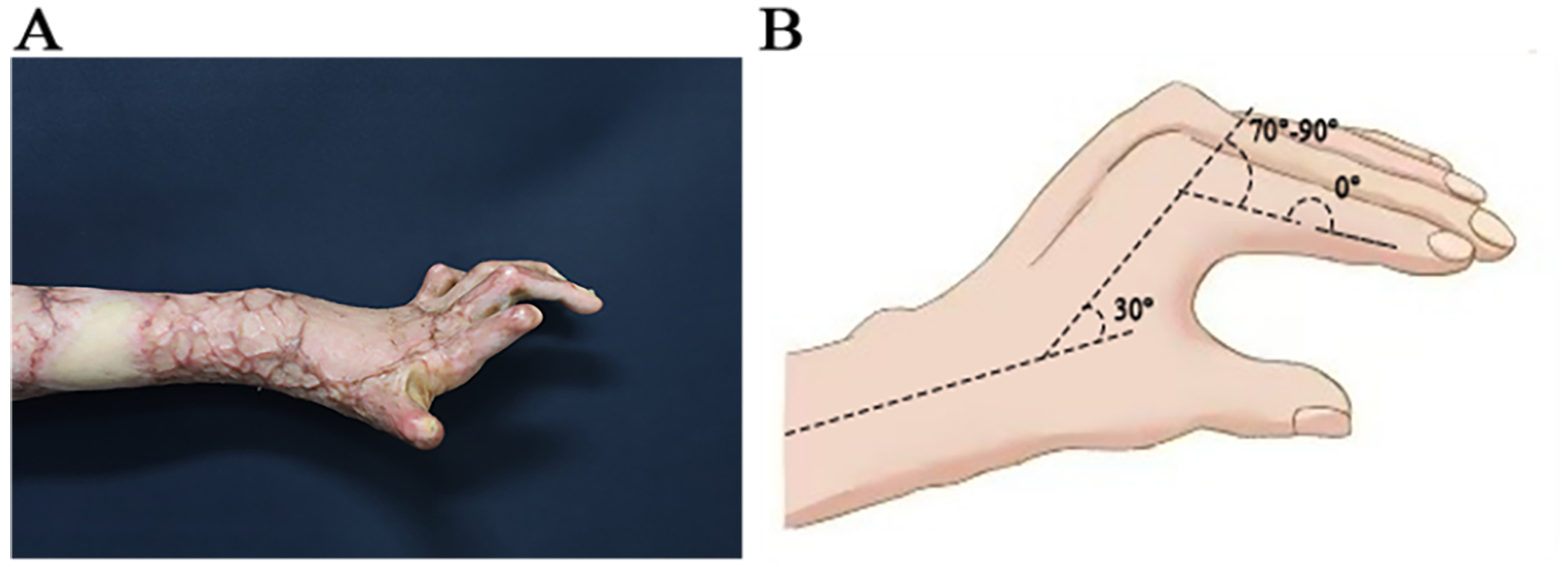
For current surgical intervention, extensive skin harvesting and graft splicing are key procedures for the correction of MCP dorsiflexion deformity, which carry substantial risks of donor site scarring, graft failure, and infection[15-17]. As illustrated in Figure 1, the resultant deformities exhibit a flexion direction diametrically opposed to the natural functional position of the hand, critically compromising operational capacity. Consequently, it highlights a pressing need to develop innovative techniques that enable an effective correction of these deformities, while minimizing surgical risks and complications - a pivotal unmet challenge in burn reconstruction.
Figure 1. Comparison of MCP joint dorsiflexion deformity and the functional hand position. (A) Lateral view of MCP dorsiflexion deformity; (B) Lateral view of the functional hand position. MCP: Metacarpophalangeal.
Currently, the surgical management of scar contracture[18] involves excision of scar tissue, release of contracted structures, and reconstruction of hand function, with the ultimate goal of improving overall functionality. Free flap transplantation and dermal stent combined with split-thickness skin grafts are representative surgical procedures in contemporary techniques, offering additional options for treating MCP joint dorsiflexion deformities. Noticeably, full-thickness skin grafting remains the most cost-effective approach. Traditional methods often necessitate extensive skin harvesting[19] and skin splicing during grafting. Extensive skin harvesting may result in significant scarring and dysfunction at the donor sites, in addition to increased surgical complexity and risk. Moreover, skin splicing during grafting may result in compromised surgical outcomes due to high susceptibility to complications such as poor skin survival, infection, and necrosis. The primary challenges associated with skin transplantation include: (1) extensive skin harvesting and donor site closure; (2) optimization of skin grafting to improve hand function; and (3) precise skin coverage without wastage or patchwork. Given these issues, there is currently a lack of a definitive surgical paradigm.
In view of the above, it underscores the necessity of developing a surgical solution that can effectively correct hand cicatricial contracture deformities while reducing surgical difficulty and risk, improving skin survival, and promoting functional recovery. To tackle these challenges, our research team devised an innovative surgical approach known as “asymmetric spindle-shaped skin flap harvesting combined with continuous Z skin grafting”. This method was found to effectively address concerns often encountered with patchwork grafting, such as extensive skin harvesting, challenging donor site closure, and suboptimal skin survival. It is possible to enhance both the functionality and aesthetics of patients’ hands, ultimately improving their overall quality of life.
TECHNIQUE: ASYMMETRIC SPINDLE SKIN HARVESTING COMBINED WITH CONTINUOUS Z SKIN GRAFTING
Indications and contraindications
Indications: Post-burn dorsiflexion deformity of the MCP joint, with or without interdigital web contracture; stable scar stage (typically > 6 months post-injury); preserved passive range of motion of the joint.
Contraindications: Poor skin quality at the donor site (abdomen) (e.g., extensive scarring, infection); severe tendon injury or joint stiffness leading to complete loss of passive range of motion; Pregnancy or lactation; severe systemic diseases that preclude surgery.
Personalized scar resection and thorough contracture scar tissue release
This procedure started with personalized resection of the hand scar and thorough scar tissue release, an initial step crucial for ensuring the success of skin grafting and recovery of hand function. Preoperatively, the formulation of a personalized resection plan primarily depended on a thorough evaluation of scar extent, thickness, contracture tension, and functional impacts. Intraoperatively, a meticulous excision was performed to remove scar tissue on the dorsal side of the hand, with special emphasis on complete eradication of the scar thickening areas and ulcers. For regions with significant restriction of joint movement, steps included careful incision of the contracture tension line along the joints, release of adhesions between tendons and joint capsules[20], and appropriate deepening of the interdigital web spaces to ensure full finger extension. In addition, efforts were made to restore as much of the normal range of motion as possible, extending incisions 0.5-1 cm beyond the margins of healthy skin to achieve continuous release and create favorable conditions for subsequent skin grafting.
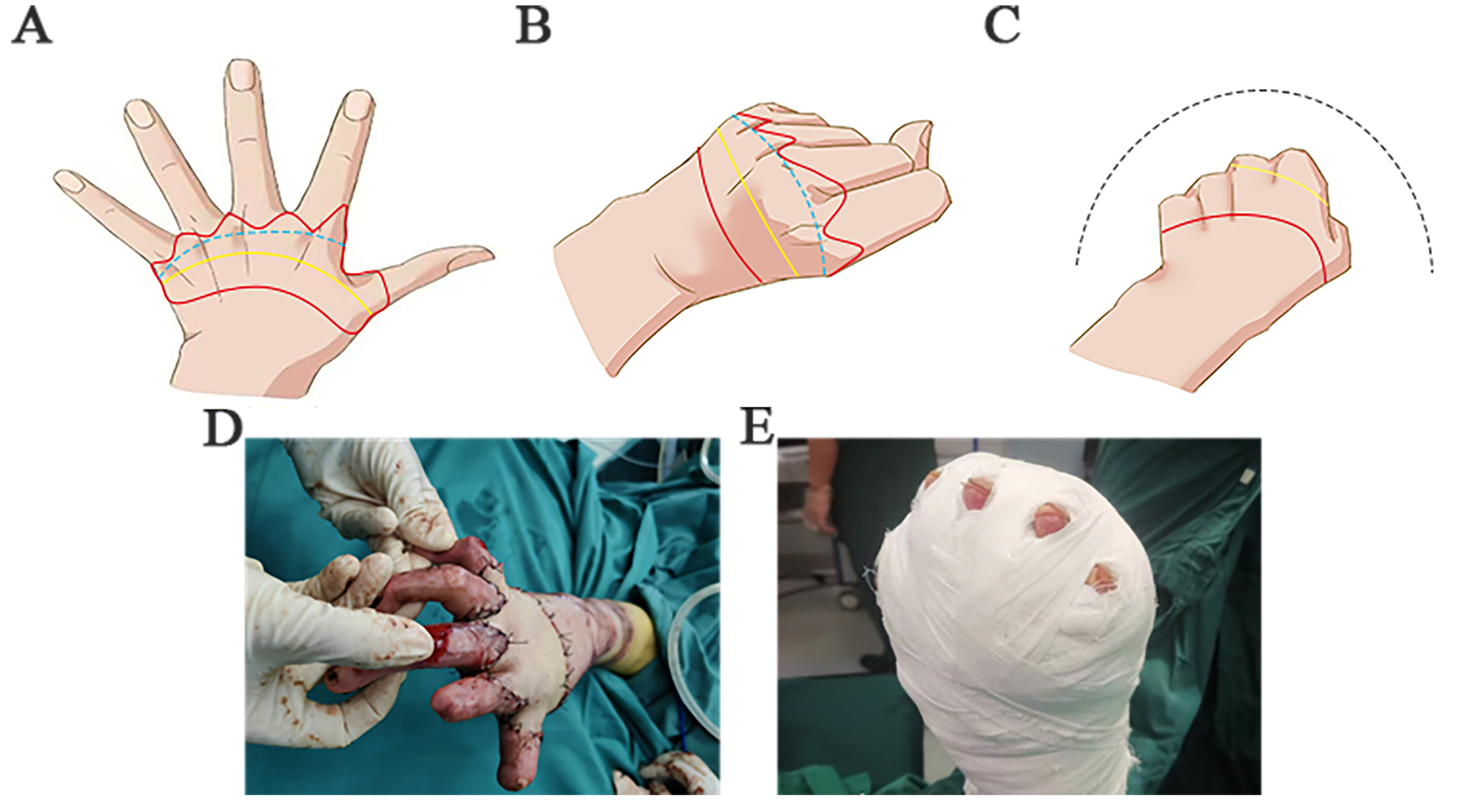
As depicted in Figure 2, after adequate scar release, the MCP joint could achieve normal flexion angles, and the edges of the recipient site naturally formed a continuous “Z” shape. This surgical design not only minimizes postoperative linear scar formation but also more effectively improves hand function.
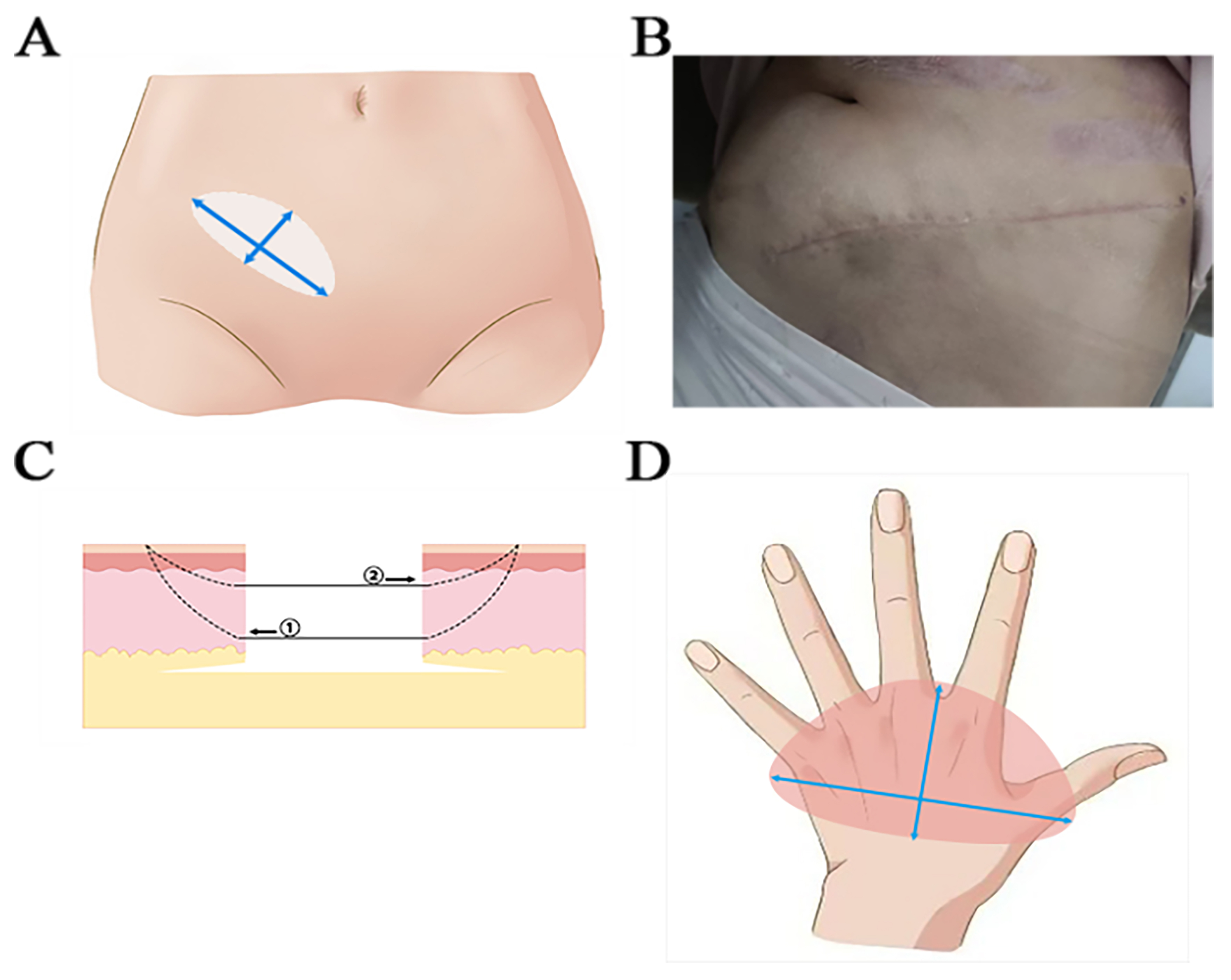
Asymmetric spindle skin harvesting combined with a super tension-reducing suture technique
Skin harvesting is a key step in surgery that directly influences the survival of subsequent skin grafts and postoperative outcomes. The abdomen, characterized by soft skin and excellent healing capacity, was recommended as the ideal donor site[21], thereby minimizing the impact on the donor site post-harvest. The long axis of the asymmetric spindle incision was designed to align as much as possible with the natural tension lines (Langer’s lines of skin tension, or the cleavage lines) of the abdominal skin (typically transverse or oblique) to facilitate wound closure with minimal tension and optimize the aesthetic effect of the donor site. During scar excision and skin grafting, it was discovered that the web area of the finger usually required a larger skin surface than the back of the hand after scar release and removal. To address this, we innovatively designed a method for asymmetric spindle-shaped skin flap harvesting. As illustrated in Figure 3, we employed an asymmetric spindle-shaped incision tailored to the specific size and shape of the recipient site. The asymmetric spindle-shaped design, in other words, the edge length of one long arc was greater than that of the other short arc, enabled a precise matching of the larger arc to the MCP joint plane, and matching of the smaller arc to the dorsal side of the hand. Through this surgical design, it would avoid: (1) the harvest of excessive skin for skin grafting (wasting skin grafts, large donor wounds); (2) limited size of the dorsal graft (the risk of finger web coverage or insufficient tension); and (3) the risk of postoperative skin graft infection and scar contracture caused by skin graft splicing. This type of incision we designed could be adjusted flexibly to meet the individual needs of different patients[8,9]. The long axis of the incision should match the longest distance between the ulnar and radial sides of the recipient site, while the short axis should extend approximately 1 cm beyond the width of the recipient site to deepen the finger web and reserve a shrinkage margin. Ultimately, it would guarantee complete coverage of the recipient site while allowing additional space for trimming and adjustment.
Figure 3. Schematic diagram of asymmetric spindle-shaped skin flap harvesting with an ultra-tension-reducing suture. (A) The skin was harvested by excision through an asymmetric spindle incision in the abdomen; (B) There were relatively few postoperative scars in the abdominal donor site after using ultra-tension-reducing suture; (C) Schematic diagram of the ultra-tension-reducing suture technique. The annotations in the picture represent the process of suturing; (D) The larger arc of the asymmetric spindle-shaped graft was utilized to reconstruct the finger web space, while the smaller arc to repair the dorsal hand.
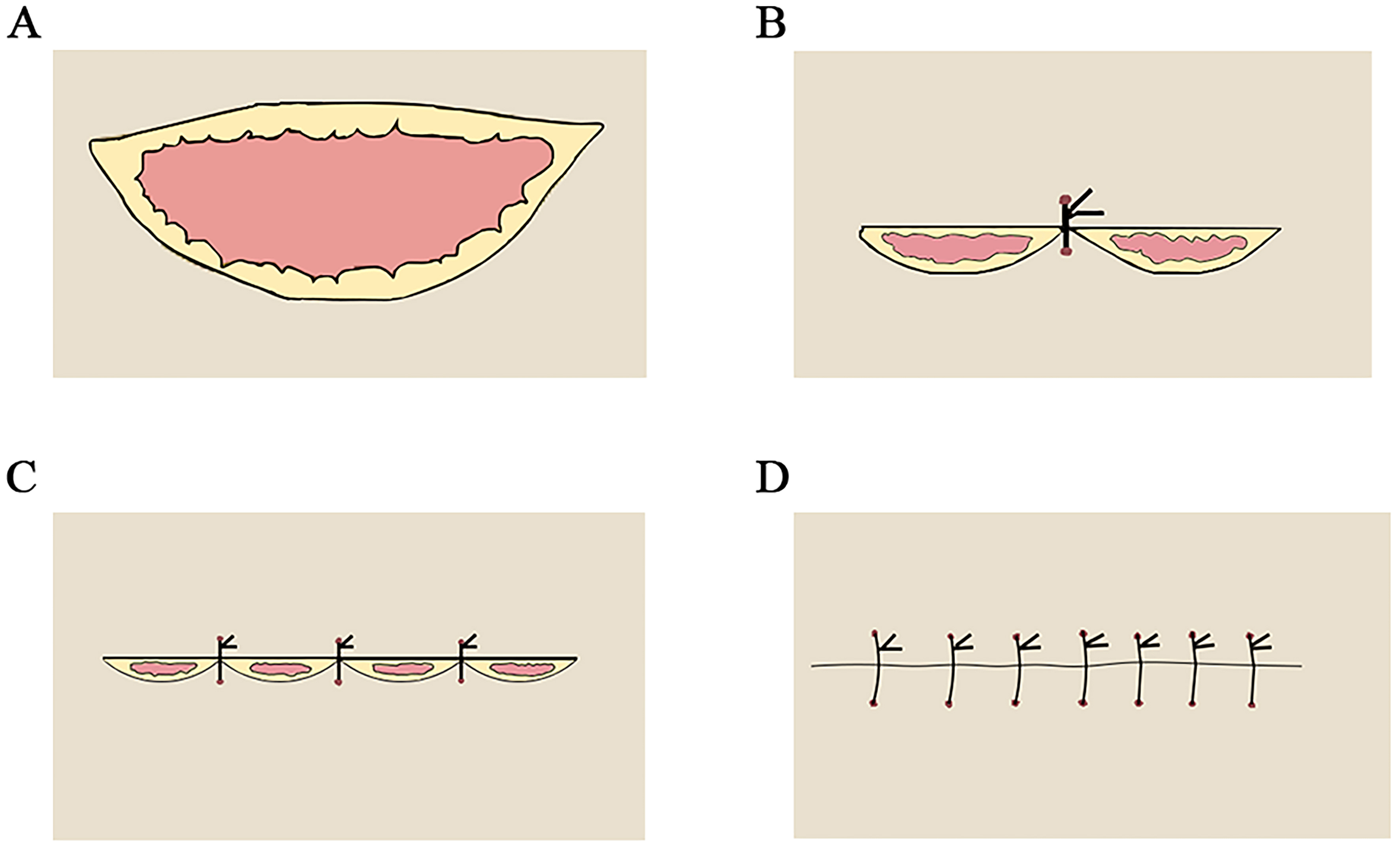
Throughout the skin harvesting, the blood vessels and nerves in the donor site should be protected cautiously to preserve the integrity of the deep vascular network. After that, the subcutaneous tissue should be properly separated from the skin margin bilaterally following proper de-fatting of the abdominal donor site. Subsequently, the ultra-tension-reducing suture technique would be employed to suture the abdominal donor site. By utilizing a “middle-middle-middle” strategy, as illustrated in Figure 4, this technique was initiated with a precise approximation of the wound center point, then sequential suturing from the center outward to bilateral midpoints, and finally, suturing the ends. Combined with adequate subcutaneous undermining and meticulous layered closure (deep dermal absorbable sutures), this technique could achieve: (1) uniform tension distribution along the entire wound; (2) precise tissue layer alignment; (3) significant reduction in wound edge tension; and (4) minimized scar formation by promoting low-tension healing and avoiding ischemia. This systematic approach is a key innovation over standard sutures (simple interrupted/continuous suture) for the closure of long and asymmetric wounds. Consequently, this technique effectively reduces tension at the donor site[22], accelerates healing, and minimizes postoperative scarring. Considering the asymmetric fusiform incision used in abdominal skin harvesting, specific techniques for suture [Figure 4] were adopted to ensure a neat wound closure, minimize scarring, and improve overall aesthetics. Specifically, the central portions of both wound edges were first sutured to ensure proper bilateral tissue alignment. Suturing then proceeded laterally from the center toward both ends until the wound was completely closed. This “middle-middle-middle” suture provided a useful strategy for avoiding tissue malalignment and scar formation, as evidenced by effective tissue alignment and maintained uniform tension throughout the wound. In case of excess skin, commonly referred to as “cat ears”, at both ends after wound closure, an oval incision was made along the base of the cat ears to facilitate subsequent layered suture of excess skin.
Figure 4. Diagram of asymmetric fusiform incision: (A) An asymmetric fusiform incision in which the lower edge exceeded the length of the upper edge; (B) Initial suture of the central portion of the wound; (C) Progressive suture of the wound from the central part toward the lateral aspects bilaterally; (D) Final appearance of the closed wound after suturing.
Continuous Z skin grafting with whole palm bandage fixation in a functional position
Skin grafting is a critical component in achieving optimal surgical outcomes. Traditional grafting faces challenges such as difficulties with graft splicing and noticeable postoperative scarring. As illustrated in Figure 5, during skin grafting, the finger web was observed to require a larger skin graft compared to the dorsal side of the hand, motivating us to utilize asymmetric spindle-shaped skin grafts. In grafting, the larger curved edge of the skin graft was strategically used to repair the web. A continuous Z-shape was designed to align with the Z-flap of the recipient site, allowing for continuous Z skin grafting along the edge. The Z-design could disperse longitudinal tension across joints and webs into smaller transverse vectors, which would contribute to reduced linear contracture forces. Meanwhile, it could expand the contact area between graft and skin of the recipient site, potentially aiding earlier vascularization and more uniform integration, and minimizing scar hypertrophy due to localized tension. In addition to enhancing the extensibility of the skin graft to prevent the recurrence of finger web contractures[20,23], this approach could also enable better adaptation to the tension at the recipient site, thereby minimizing the risk of linear scarring post-surgery. During trimming and suturing, the tension-elastic properties of the skin were carefully considered to ensure the graft was positioned naturally without undue tension, thereby allowing it to adapt to joint motion. Following appropriate trimming, the skin graft was sutured intermittently to the wound edges to ensure a natural stretching, avoiding any undue tension or twisting. Upon grafting, the long axis of the skin graft was aligned with the plane of the MCP joint when the hand was positioned functionally or in a clenched fist, thereby maximizing its release. Postoperatively, the entire palm was subjected to comprehensive bandaging while maintaining the functional position[2,23] (wrist in 20° dorsiflexion, MCP joint in 70° flexion, and the interphalangeal joint in slight flexion). This positioning was crucial to ensure optimal healing of the skin graft and accelerate hand function recovery. To support the rehabilitation of hand function, after two weeks, the patient was encouraged to engage in appropriate functional exercises after the removal of the bandages.
Figure 5. Continuous Z skin grafting at the edge, along with bandaging in functional position and immobilization of the entire palm. (A-C) Repair of the finger web with the larger, curved side of the skin, and suture of the recipient site in a continuous Z-shape to ensure smooth and optimal release of the skin; (D) Uniform stretching of the skin without twisting or pulling after the completion of skin grafting; (E) Bandaging of the functional position of the hand and immobilization following the surgery.
RESULTS
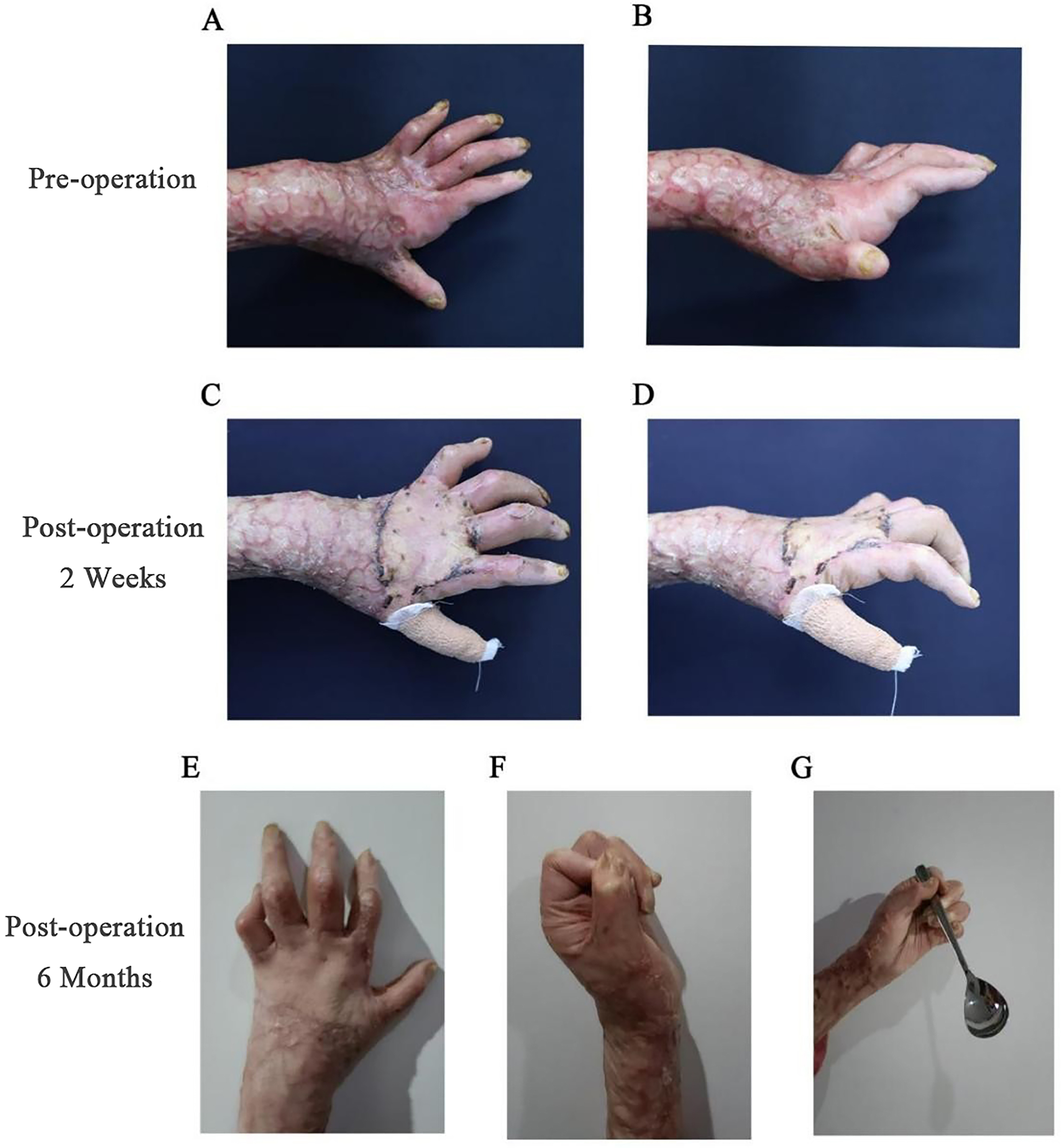
As displayed in Figure 6, postoperative follow-up revealed a significant improvement in the dorsiflexion deformity of the MCP joint, and considerable recovery of the hand function. All patients were satisfied with both the appearance and functionality of their hands. There was no wastage during skin harvesting or need for skin graft splicing, and the skin grafts integrated well without complications such as infection or necrosis.
Figure 6. Significant improvement in the MCP dorsiflexion deformity following the operation. (A and B) The appearance of a “claw hand” of the deformity preoperatively; (C and D) Slight improvement of the dorsiflexion deformity of the MCP joint 2 weeks after the surgery, characterized by smooth skin and favorable healing conditions; (E-G) Restoration of normal functionality (fist gripping and holding) of the hand joint, and the observation of minimal scar on the hand 6 months after the surgery. MCP: Metacarpophalangeal.
DISCUSSION
Our research team designed and developed an innovative and efficient surgical strategy termed “Asymmetric spindle skin harvesting combined with continuous Z skin grafting” to correct dorsiflexion deformities of the MCP joint in burn patients. Through careful surgical implementation, this technique not only addresses the primary issues of scar excision and joint contracture release but also enhances hand function and appearance by optimizing skin harvesting and grafting methods. Additionally, it helps minimize trauma and scar formation at the donor site.
In our opinion, this approach offers several advantages. To be specific, our technique avoids splicing entirely. Traditionally, the conventional use of full-thickness grafting requires splicing[15-17], carrying risks of infection, necrosis, suture line dehiscence, and hypertrophic scarring at junctions. Meanwhile, this technique incorporates ultra-tension-reducing suture to minimize donor site complications, and the continuous Z skin grafting to reduce the risk of linear scar contracture at the MCP joint plane.
Its specific advantages may include the following aspects. The first strength is the significant improvement in hand function through personalized scar resection and effective contracture release. Besides the removal of scar tissues, individualized scar resection can ensure adequate release of joint contractures. During skin grafting, the degree of release can be maximized when the long axis of the skin graft aligns with the plane of the MCP joint. This strategic design can remarkably improve patients’ hand function and their quality of life, while providing individualized surgical treatment and hence the optimal therapeutic effect for patients with varied conditions.
The second benefit lies in minimizing damage to the donor site, as supported by the combined application of asymmetric fusiform incision skin harvesting and a super tension-relieving suture technique. The asymmetric fusiform incision is specifically designed for skin harvesting to make the area of skin harvesting more in line with the natural tension line of the skin and reduce the tension at the donor site. Furthermore, the use of super tension-relieving suture can further reduce the tension of the wound, significantly decrease scar formation, and lower the risk of complications at the donor site.
Last but not least, the third advantage lies in the improved utilization of skin grafts, resulting from the accurate design of skin harvesting and the continuous Z skin grafting. The asymmetric fusiform skin harvesting method enables full coverage of the recipient site, with extra margin for trimming and adjustment. Simultaneously, the continuous Z skin grafting eliminates the complexity of traditional skin graft splicing and enables the graft to better accommodate the tension of the recipient site. Ultimately, this approach minimizes graft wastage and maximizes graft survival, thereby ensuring optimal use of the harvested skin.
Indeed, we harvested skin from the abdominal region (the donor site) for its favorable properties. Notably, the core principles of the technique - asymmetric spindle design, continuous Z skin grafting, and super tension-reducing suturing - are generalizable and offer advantages such as reduced contracture formation and improved donor site healing. While applicable to other donor sites, the abdomen remains the preferred region.
The residual joint stiffness observed in the early postoperative period (e.g., at 6 months) is multifactorial and may result from: (1) temporary limitations due to postoperative pain, swelling, and immobilization; (2) patient compliance with rehabilitation protocols. Based on our quantitative findings, most patients showed continued improvement in range of motion at 6 months and 1 year follow-up, particularly when engaged in consistent, specialized functional exercises (initiated 2 weeks post-bandage removal, emphasizing active/passive motion). This highlights the significance of ongoing, professional rehabilitation in achieving optimal functional recovery.
As a technical note focused primarily on the surgical technique, this report has certain inherent limitations. The description is based on our experience with a small cohort (n = 12) and a follow-up duration ranging from 2 weeks to 1 year. Consequently, it lacks sufficient longitudinal data to comprehensively assess long-term outcomes (> 5 years). Future larger-scale studies or prospective investigations will be essential to confirm the broader applicability and sustained benefits of this innovative strategy. Moreover, although postoperative improvements in MCP joint mobility and hand function were clinically apparent, a systematic quantification of functional metrics such as range of motion and standardized scoring was beyond the scope of this initial report. These outcome measures are currently being analyzed in a larger patient group and will be presented in future publications. Despite the limitations inherent to the technical note format, the described technique demonstrates promising feasibility and innovation. Future efforts will focus on precise metric analysis, particularly concerning the dimensions of the released interdigital web spaces and their correlation with functional improvement, to further refine and substantiate this approach.
CONCLUSION
In conclusion, “Asymmetric Spindle Skin Harvesting combined with continuous Z skin grafting at the edge” may be an effective surgical solution for correcting MCP joint dorsiflexion deformities in burn patients. When paired with meticulous surgical execution and proactive postoperative rehabilitation, this approach can significantly enhance both hand function and appearance. It offers multiple clinical benefits, including minimized donor site damage, more efficient use of skin grafts, enhanced functional outcomes, and reduced postoperative scar formation[20,23,24]. Our clinical experience with 12 patients supports the safety and efficacy of this novel strategy for treating burn-related hand contracture deformities. In the future, we anticipate further innovation in surgical and rehabilitation techniques to improve outcomes and offer valuable references for practitioners in the fields of Burn and Plastic Surgery.
DECLARATIONS
Authors’ contributions
Substantial contributions to the conception and design of the study: Wang Y, Li P, Tang D, Qiu W
Data acquisition, as well as administrative, technical, and material support: Dong L, Lin Q
Availability of data and materials
Raw image data cannot be shared publicly due to patient privacy protections. De-identified quantitative datasets are available from the corresponding author upon reasonable request, subject to ethics committee approval and executed data use agreements.
Financial support and sponsorship
This research was financially supported by the National Natural Science Foundation of China Youth Program (Grant No. 82302818).
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Approved by the Ethics Committee of the General Hospital of Central Theater Command [Approval No. (2025)143-01], with written informed consent obtained from all patients prior to the study.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2025.
REFERENCES
1. Klifto KM, Yesantharao PS, Dellon AL, Hultman CS, Lifchez SD. Chronic neuropathic pain following hand burns: etiology, treatment, and long-term outcomes. J Hand Surg Am. 2021;46:67.e1-9.
2. Afifi AM, Mahboub TA, Ibrahim Fouad A, Azari K, Khalil HH, McCarthy JE. Active range of motion outcomes after reconstruction of burned wrist and hand deformities. Burns. 2016;42:783-9.
3. Gupta S, Mahmood U, Gurung S, et al. Burns in Nepal: a population based national assessment. Burns. 2015;41:1126-32.
4. Corlew DS, McQueen KA. International disease burden of hand Burns: perspective from the global health arena. Hand Clin. 2017;33:399-407.
5. van der Vlies CH, de Waard S, Hop J, et al; Dutch Burn Repository R3 Group. Indications and predictors for reconstructive surgery after hand burns. J Hand Surg Am. 2017;42:351-8.
6. Germann G. Hand reconstruction after burn injury: functional results. Clin Plast Surg. 2017;44:833-44.
8. Chen K, Henn D, Januszyk M, et al. Disrupting mechanotransduction decreases fibrosis and contracture in split-thickness skin grafting. Sci Transl Med. 2022;14:eabj9152.
9. Bergus K, Barash B, Justice L, et al. Dermal substrate application in the treatment of pediatric hand burns: clinical and functional outcomes. Int J Burns Trauma. 2023;13:204-13.
10. Hop MJ, Langenberg LC, Hiddingh J, et al. Reconstructive surgery after burns: a 10-year follow-up study. Burns. 2014;40:1544-51.
11. Ergani HM, Yalçın Topçuoğlu E, Yaşar B, et al. Physical medicine applications in hand burns: treatment or rehabilitation. J Burn Care Res. 2024;45:98-103.
12. Kalra GS, Gupta S, Kalra S. Long arm double asymmetrical sliding flaps: a technique to treat flexion contractures of digits. J Hand Surg Am. 2022;47:294.e1-4.
13. Woo SH, Seul JH. Optimizing the correction of severe postburn hand deformities by using aggressive contracture releases and fasciocutaneous free-tissue transfers. Plast Reconstr Surg. 2001;107:1-8.
14. Davami B, Pourkhameneh G. Correction of severe postburn claw hand. Tech Hand Up Extrem Surg. 2011;15:260-4.
15. Bhattacharya S. Avoiding unfavorable results in postburn contracture hand. Indian J Plast Surg. 2013;46:434-44.
16. Lee A, Wang Y, Nadarajah CC, Lipner SR. Cross-sectional analysis of national electronic injury surveillance system for burn injuries presenting to United States emergency departments 2000-2018. Burns. 2022;48:1347-54.
18. Fufa DT, Chuang SS, Yang JY. Prevention and surgical management of postburn contractures of the hand. Curr Rev Musculoskelet Med. 2014;7:53-9.
19. Alsaif A, Karam M, Hayre A, Abul A, Aldubaikhi A, Kahlar N. Full thickness skin graft versus split thickness skin graft in paediatric patients with hand burns: systematic review and meta-analysis. Burns. 2023;49:1017-27.
20. Grishkevich VM. Flexion contractures of fingers: contracture elimination with trapeze-flap plasty. Burns. 2011;37:126-33.
21. Yongwei P, Jianing W, Junhui Z, Guanglei T, Wen T, Chun L. The abdominal flap using scarred skin in the treatment of postburn hand deformities of severe burn patients. J Hand Surg Am. 2004;29:209-15.
22. Morton JD. Defining the role of secondary intention healing in full-thickness lid margin defects. Plast Reconstr Surg. 2016;138:95e-103.
23. Slater ED, James AJ, Hill JB. Optimizing outcomes in the management of the burned hand. Clin Plast Surg. 2024;51:539-51.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Copyright
Data & Comments
Data


















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at [email protected].