Laparoscopic hepaticojejunostomy for the treatment of bile duct injuries in difficult scenarios (with video)
Abstract
Open Roux-en-Y hepaticojejunostomy (RYHJ) is the treatment of choice for bile duct injuries (BDI) sustained during laparoscopic cholecystectomy. Although in recent years the mini-invasive approach has been explored at expert centers, laparoscopic RYHJ for challenging surgical scenarios has rarely been attempted. We herein report two cases of RYHJ for BDI in highly complex surgical scenarios, such as right posterior BDI or failure of previous repairs, with special emphasis on the technical aspects through the embedded videos. The first was an intraoperative repair in a 55-year-old female who suffered a Strasberg type C (transection of the aberrant right hepatic duct) thermal lesion. The second was an iterative repair in a 54-year-old female with a history of a Strasberg type E1 lesion (injury of the main hepatic duct more than 2 cm from the confluence) that had been repaired intraoperatively with an end-to-end anastomosis over a T-tube nine months before referral. Both patients had an uneventful recovery and were discharged four and five days after surgery. After 2.5 and 4 years of follow-up, both patients are asymptomatic and have normal imaging and laboratory tests. To our knowledge, there is no other report in the literature regarding intraoperative laparoscopic right posterior RYHJ for BDI. Laparoscopic RYHJ for BDI repair in the hands of expert laparoscopic biliary surgeons is feasible and safe, even in very challenging surgical scenarios, as herein reported, offering the benefits of mini-invasive surgery. Future high-quality and long-term comparative studies are necessary to elucidate its potential superiority against the standard open approach.
Keywords
INTRODUCTION
Despite the accumulated experience and technical refinements directed to increase the safety of laparoscopic cholecystectomy (LC), there has not been a significant reduction in the incidence of bile duct injuries (BDI) in the past decades[1-3]. There is consensus in the scientific community that this serious complication must be managed at tertiary specialized centers in a multidisciplinary fashion[1,2]. Although many bile leaks and injuries can be managed successfully by endoscopists and interventional radiologists, the best long-term results are obtained with definitive surgical repair[4]. Among surgical repairs, open Roux-en-Y hepaticojejunostomy (RYHJ) is the treatment of choice, with > 90% success rate in expert hands[4-6]. In addition to a higher success rate, surgical repair has even been associated with improved survival and reduced cumulative cost compared with endoscopic management[7]. Although in recent years the mini-invasive approach has been explored at expert centers with encouraging results, laparoscopic RYHJ for challenging surgical scenarios, such as right posterior BDI or failure of previous repairs, has rarely been attempted[8-11].
CASES PRESENTATIONS AND SURGICAL TECHNIQUE
We herein report two cases of RYHJ for BDI in highly complex surgical scenarios, with special emphasis on the technical aspects through the embedded videos. The first was an intraoperative repair in a patient who suffered a Strasberg type C thermal lesion. The second was an iterative repair after the failure of intraoperative end-to-end anastomosis in a patient with a history of a Strasberg type E1 lesion.
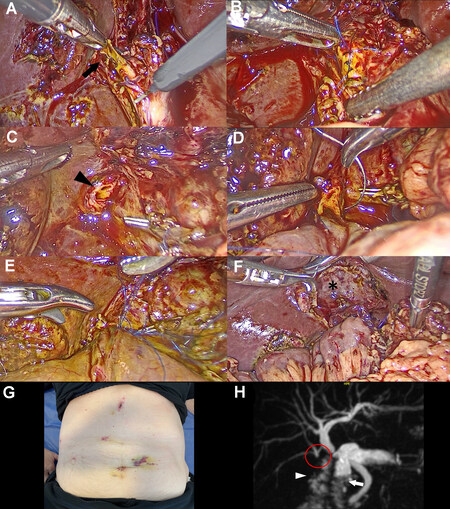
Case A: A 55-year-old female was admitted for elective LC due to symptomatic gallstones disease. During surgery, while dissecting the posterior aspect of the Calot’s triangle, the operating surgeon committed a partial thermal lesion of the right posterior duct (Strasberg type C), which drained separately in the main hepatic duct as an anatomic variant. A hepato-pancreatic-biliary (HPB) surgery specialist was called into the operating room for immediate management of the BDI. This case was particularly challenging because the patient had a previous open Roux-en-Y gastric bypass, and the anastomosis had to be performed over a very small (2 mm) right posterior duct [Figure 1 and supplementary Video 1]. After confirming the injury and biliary anatomy through an intraoperative cholangiogram, the cholecystectomy was completed, and the burned aberrant duct was resected up to healthy tissue. Distally, the resection ended at the level of the common hepatic duct, and proximally it went up to the level of the bifurcation of the third order ducts for segments 6 and 7. The resulting lateral defect in the common hepatic duct was closed with interrupted stitches of a 6/0 monofilament suture. Later, a 12 mm trocar was added to the classic American technique of LC in the left flank for the biliodigestive repair. After performing a new stapled Roux limb distal to the previous one, the jejunal loop was ascended to the hepatic hilum through the retro-colic para-duodenal route in order to facilitate a tension-free anastomosis. Due to the very small caliber of the proximal injured duct, it was decided to perform a right posterior RYHJ with four separate rhombus-shaped running sutures using a 6/0 monofilament material. This is a very important technical tip to avoid stenosis of very small ducts when performing running sutures. After fixing the jejunal loop with two stitches on each side of the anastomosis above the mesocolon, two drains were placed in the anterior and posterior aspects of the RYHJ. The patient had an uneventful recovery and was discharged four days after surgery. After 2.5 years of follow-up, she is asymptomatic, with normal imaging and laboratory tests.
Figure 1. Case A: (A) Partial thermal lesion of the right posterior duct (black arrow). (B) Closure of the lateral defect in the common hepatic duct with interrupted stitches. (C) Proximal stump of the aberrant right posterior duct after resection up to the level of the bifurcation for segment 6 and 7 ducts (black arrowhead). (D) Right posterior RYHJ. (E) The end-to-side RYHJ is completed. (F) Final view of the retro-colic jejunal loop and the gallbladder fossa (asterisk) after cholecystectomy. (G) Postoperative view of the abdomen with the previous open scar and the trocar disposition for the biliodigestive repair. (H) One year after surgery, a magnetic resonance cholangiopancreatography shows a patent right posterior RYHJ (red circle) without dilatation of the intrahepatic biliary tree. The jejunal loop (white arrowhead) is seen next to the duodenum (white arrow). RYHJ: Roux-en-Y hepaticojejunostomy.
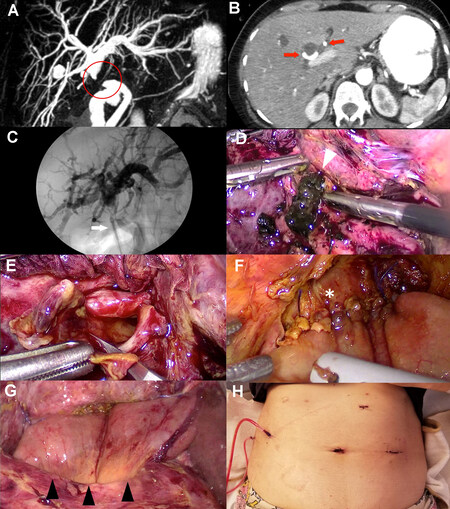
Case B: A 54-year-old female with a history of a Strasberg type E1 lesion that had been repaired intraoperatively with an end-to-end anastomosis over a T-tube nine months before referral presented with cholestasis. She developed severe stenosis at the level of the previous end-to-end repair with intrahepatic biliary dilatation, and after the failure of endoscopic treatment, it was decided to perform a biliodigestive anastomosis as definitive treatment [Figure 2 and supplementary Video 2]. A preoperative CT scan ruled out an associated vascular injury. This case had multiple adhesions caused by the previous open repair and a consolidated fibrous process within the portal pedicle. After releasing multiple adhesions from the previous open surgery, an intraoperative cholangiography through direct puncture of the suspected main bile duct (MBD) with a 30 G yellow needle was performed to accurately locate the dilated proximal bile duct in the fibrotic pedicle. The proximal dilated bile duct was opened, and the diseased extrahepatic bile duct was resected with scissors up to healthy well-perfused tissue below the biliary confluence. Finally, an end-to-side RYHJ was performed with two separate 4/0 running sutures of a monofilament material, first the posterior wall from left to right and then the anterior wall in the same fashion. Two fixing stitches were placed on each side of the hepaticojejunostomy between the bowel and the liver to release tension in the anastomosis and avoid any twisting of the jejunal loop. The patient recovered successfully without complications and was discharged five days after surgery. After four years of follow-up, she is asymptomatic, with normal imaging and laboratory tests.
Figure 2. Case B: (A) Preoperative magnetic resonance cholangiopancreatography shows intrahepatic biliary dilatation with the MBD stenosis (red circle) at the level of the previous end-to-end repair. (B) An abdominal contrast-enhanced CT scan shows a patent right and left hepatic artery (red arrows). (C) Direct puncture intraoperative cholangiography with a 30 G needle (white arrow). (D) The proximal dilated bile duct is opened, and a large amount of biliary sludge (white arrowhead) is drained. (E) The diseased extrahepatic bile duct is resected with scissors up to healthy well-irrigated tissue below the biliary confluence. (F) End-to-side RYHJ (asterisk). (G) Final view of the RYHJ and the retro-colic para-duodenal jejunal loop (black arrowheads). (H) Postoperative view of the abdomen with the previous open scar and the trocar disposition for the biliodigestive repair. RYHJ: Roux-en-Y hepaticojejunostomy; MBD: main bile duct.
DISCUSSION
Bile duct injuries are still among the most serious iatrogenic surgical complications encountered by general surgeons, with a profound impact on patients’ quality of life, health care costs, and surgeon’s well-being and career that can be devastating[12-15]. A recent survey performed by the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) showed that nearly half (47%) of surgeons with an average time in the practice of 16.1 years experienced a BDI during a LC in their career, the majority of whom (61.2%) had fellowship training, with almost one out of five having experienced multiple BDIs[16]. Interestingly, the majority of the surveyed surgeons (58%) felt that BDIs could be repaired laparoscopically and 25% had done so in practice[16]. Despite the relative lack of haptic perception in the minimally invasive approach, invoked by some skeptics as a handicap of the laparoscopic approach, increasing retrospective data suggest that minimally invasive repair is feasible, safe, and at least non-inferior to open surgery in properly selected patients[8-11, 17-22]. Which of the two available minimally invasive techniques is the best, robotic or laparoscopic, is still a matter of debate[23], with a recent study by Cuendis-Velázquez et al. showing similar results regarding safety and efficacy in attaining primary anastomotic patency[11]. However, the robotic technology offers attractive advantages by providing a stable camera with three-dimensional imaging, elimination of physiologic tremor, enhanced dexterity, and allowing an ergonomic operating position, all of which are prized benefits for the surgeon when performing complex surgical procedures such as BDI repairs[23]. Table 1 summarizes the most important features of the published experiences regarding laparoscopic RYHJ for BDI repair. The largest published series to date of laparoscopic RYHJ for BDI repair, with 40 patients, found a 27.5% overall morbidity rate and no mortality, with a primary patency rate of 92.5% during a median follow-up of 49 months[11]. These results compare favorably with large published series of open repairs at expert centers[4,5,24]. In addition, a recent retrospective study by Javed et al., comparing 29 laparoscopic bilio-enteric anastomoses with 34 patients receiving open repairs, found significantly less morbidity (20% vs. 38%) and intraoperative blood loss (50 mL vs. 200 mL) and shorter time to oral intake (2 vs. 4 days), and hospital stay (6 vs. 8 days) in the laparoscopic repair group, while there were no significant differences regarding operative time and success rate[22]. Despite the absence of high-quality evidence to conclude in favor of minimally invasive approaches, the fact that expert centers are increasingly performing and favoring the minimally invasive repair of BDI is also supported by the fact that minimally invasive repair replicates the fundamental surgical principles for the long-term success of bile duct repairs established in open surgery[25], adding the advantages of laparoscopy for the surgeon (high-definition magnification) and patient (enhanced recovery).
Published series of laparoscopic Roux-en-Y hepaticojejunostomy for BDI repair
| Author | Year | Country | N | Morbidity | Mortality | Success rate |
| Chowbey et al.[18] | 2005 | India | 10 | 25% | 0% | 75% |
| Palermo et al.[19] | 2011 | USA | 1 | 0% | 0% | 100% |
| Chen et al.[20] | 2013 | China | 3 | 66% | 0% | 100% |
| Cuendis-Velázquez et al.[9] | 2016 | Mexico | 29 | 31% | 0% | 96% |
| Dokmak et al.[8] | 2017 | France | 3 | 0% | 0% | 100% |
| Cuendis-Velázquez et al.[11] | 2019 | Mexico | 40 | 27.5% | 0% | 92.5% |
| Goméz et al.[17] | 2020 | Espain | 20 | 10% | 0% | 100% |
| Sahoo et al.[21] | 2021 | India | 16 | 50% | 0% | 100% |
| Javed et al.[22] | 2021 | India | 13 | 20.7% | 0% | 96.5% |
In terms of the technical aspects of our technique, some points should be discussed. Although in one of our cases, in whom a delayed repair was being performed, we chose to puncture and dye the biliary tree for an intraoperative “radiographic” cholangiography to better identify the main bile duct, another alternative could be the more recently developed indocyanine green near-infrared “fluorescent” cholangiography, which is widely spreading in clinical practice to delineate biliary anatomy[26]. With regards to our duct-to-jejunum anastomosis, while we used running sutures of a monofilament non-absorbable material, equally good results have been obtained by other surgeons using interrupted stitches and multifilament sutures, as observed in open surgery[8,9,21,22]. Finally, some surgeons have described the use of transanastomotic stents after BDI repair up to nine months after surgery to relieve intraductal pressure and maintain a patent anastomosis[27]. However, there have been some reports of complications related to its use, with no clear benefit[9]. It is nowadays generally accepted that transanastomotic stents may have a role only in selected cases, mostly when unhealthy and small ducts are being anastomosed[9]. In our center, we only use transanastomotic stents if the patient had a previous percutaneous biliary drainage still in place, which is usually removed if no complications are encountered between two and four weeks after surgery, depending on the degree of tract formation.
In line with previous reports, the present manuscript highlights the feasibility and safety of minimally invasive laparoscopic repair of BDI, even for complex immediate or late repairs in very challenging surgical scenarios. In addition, to our knowledge, this is the first report in the literature regarding intraoperative repair of BDI by laparoscopic right posterior RYHJ. Given the associated technical complexity, laparoscopic RYHJ for BDIs is still extraordinarily unusual and reserved mostly for a few highly specialized HPB centers, as shown in Table 1. Therefore, the main objective of the accompanying videos is to highlight the key aspects of our RYHJ technique, in order to help other experienced surgeons around the world incorporate this technique and reproduce it in a safe and effective manner. Our service started performing laparoscopic repairs for patients with BDIs on a routine basis in January 2018, after the senior author of this manuscript (FA), who performed the procedures, moved from a high-volume HPB center with an already completed learning curve in this type of repairs as well as laparoscopic hepaticojejunostomies for other diseases (choledochal cysts, cholangiocarcinomas, pancreaticoduodenectomies, and radical cholecystectomies for cancer and recurrent bile duct stones). It is therefore recommended that, before embarking on highly complex repairs, such as those presented in this manuscript, surgeons should start performing laparoscopic RYHJ in less complex cases for other benign diseases such as choledochal cysts or recurrent bile duct stones. In terms of patient selection, although this is an evolving field and selection criteria might change over time, we consider that during the initial steps of the learning curve, those patients with a dilated common bile duct, with a Bismuth type 1 biliary stricture (in which an intact biliary confluence and a long stump of the bile duct is available), and no associated vascular injury are the most appropriate candidates for this approach.
CONCLUSION
Laparoscopic RYHJ for BDI repair in the hands of expert laparoscopic biliary surgeons is feasible and safe, even in very challenging surgical scenarios, as herein reported, offering the benefits of mini-invasive surgery. Future high-quality and long-term comparative studies are necessary to elucidate its potential superiority against the standard open approach.
DECLARATIONS
AcknowledgmentsWe thank Ms. Zara Elizabeth Jestadt for kindly giving voice to the videos attached to this article.
Authors’ ContributionsConception and design: Doniquian AM, Alvarez FA
Acquisition, analysis, and interpretation of data: Pinsak A, Gielis M, Alvarez FA, Viscido G
Manuscript drafting and editing: Pinsak A, Gielis M, Doniquian AM, Alvarez FA, Viscido G
Final approval of manuscript: Pinsak A, Gielis M, Doniquian AM, Alvarez FA, Viscido G
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflict of InterestAll authors declared that there are no conflicts of interest for this article.
Ethical approval and consent to participateNot applicable.
Consent for publicationA written informed consent for publication was obtained.
Copyright© The Author(s) 2022.
Supplementary MaterialsREFERENCES
1. Brunt LM, Deziel DJ, Telem DA, et al. ; the Prevention of Bile Duct Injury Consensus Work Group. Safe cholecystectomy multi-society practice guideline and state of the art consensus conference on prevention of bile duct injury during cholecystectomy. Ann Surg 2020;272:3-23.
2. Iwashita Y, Hibi T, Ohyama T, et al. Delphi consensus on bile duct injuries during laparoscopic cholecystectomy: an evolutionary cul-de-sac or the birth pangs of a new technical framework? J Hepatobiliary Pancreat Sci 2017;24:591-602.
3. Alvarez FA, de Santibañes M, Palavecino M, et al. Impact of routine intraoperative cholangiography during laparoscopic cholecystectomy on bile duct injury. Br J Surg 2014;101:677-84.
4. Pitt HA, Sherman S, Johnson MS, et al. Improved outcomes of bile duct injuries in the 21st century. Ann Surg 2013;258:490-9.
5. Sicklick JK, Camp MS, Lillemoe KD, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann Surg 2005;241:786-92; discussion 793.
6. de'Angelis N, Catena F, Memeo R, et al. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg 2021;16:30.
7. Fong ZV, Pitt HA, Strasberg SM, et al. California Cholecystectomy Group. Diminished survival in patients with bile leak and ductal injury: management strategy and outcomes. J Am Coll Surg 2018;226:568-76.e1.
8. Dokmak S, Amharar N, Aussilhou B, et al. Laparoscopic repair of post-cholecystectomy bile duct injury: an advance in surgical management. J Gastrointest Surg 2017;21:1368-72.
9. Cuendis-Velázquez A, Morales-Chávez C, Aguirre-Olmedo I, et al. Laparoscopic hepaticojejunostomy after bile duct injury. Surg Endosc 2016;30:876-82.
10. Guerra F, Coletta D, Gavioli M, Coco D, Patriti A. Minimally invasive surgery for the management of major bile duct injury due to cholecystectomy. J Hepatobiliary Pancreat Sci 2020;27:157-63.
11. Cuendis-Velázquez A, Trejo-Ávila M, Bada-Yllán O, et al. A new era of bile duct repair: robotic-assisted versus laparoscopic hepaticojejunostomy. J Gastrointest Surg 2019;23:451-9.
12. O'Brien S, Wei D, Bhutiani N, et al. Adverse outcomes and short-term cost implications of bile duct injury during cholecystectomy. Surg Endosc 2020;34:628-35.
13. Booij KAC, de Reuver PR, van Dieren S, et al. Long-term impact of bile duct injury on morbidity, mortality, quality of life, and work related limitations. Ann Surg 2018;268:143-50.
14. Halle-Smith JM, Marudanayagam R, Mirza DF, Roberts KJ. Long-term outcomes of delayed biliary strictures following cholecystectomy. HPB (Oxford) 2022;24:209-16.
15. Tebala GD, Nuzzo G. Iatrogenic biliary injury during cholecystectomy: critical review of a historical case and its political consequences. Dig Surg 2021;38:91-103.
16. Fletcher R, Cortina CS, Kornfield H, et al. Bile duct injuries: a contemporary survey of surgeon attitudes and experiences. Surg Endosc 2020;34:3079-84.
17. Goméz D, Cabrera LF, Pedraza-Ciro M, Mendoza A, Pulido J. Laparoscopic Roux-en-Y hepaticojejunostomy reconstruction after iatrogenic bile duct injury: case series report. Cir Cir 2020;88:608-16.
18. Chowbey PK, Soni V, Sharma A, Khullar R, Baijal M. Laparoscopic hepaticojejunostomy for biliary strictures: the experience of 10 patients. Surg Endosc 2005;19:273-9.
19. Palermo M, Trelles N, Gagner M. Laparoscopic revisional hepaticojejunostomy for biliary stricture after open repair following common bile duct injury: a case report. Surg Innov 2011;18:105-9.
20. Chen D, Zhu A, Zhang Z. Total laparoscopic Roux-en-Y cholangiojejunostomy for the treatment of biliary disease. JSLS 2013;17:178-87.
21. Sahoo MR, Ali MS, Sarthak S, Nayak J. Laparoscopic hepaticojejunostomy for benign biliary stricture: A case series of 16 patients at a tertiary care centre in India. J Minim Access Surg 2022;18:20-4.
22. Javed A, Shashikiran BD, Aravinda PS, Agarwal AK. Laparoscopic versus open surgery for the management of post-cholecystectomy benign biliary strictures. Surg Endosc 2021;35:1254-63.
23. Giulianotti PC, Quadri P, Durgam S, Bianco FM. Reconstruction/repair of iatrogenic biliary injuries: is the robot offering a new option? Ann Surg 2018;267:e7-9.
24. Iannelli A, Paineau J, Hamy A, Schneck AS, Schaaf C, Gugenheim J. Primary versus delayed repair for bile duct injuries sustained during cholecystectomy: results of a survey of the Association Francaise de Chirurgie. HPB (Oxford) 2013;15:611-6.
25. Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM. “Sideways”: results of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg 2009;249:426-34.
26. Pesce A, Piccolo G, Lecchi F, Fabbri N, Diana M, Feo CV. Fluorescent cholangiography: an up-to-date overview twelve years after the first clinical application. World J Gastroenterol 2021;27:5989-6003.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Pinsak A, Gielis M, Viscido G, Doniquian AM, Alvarez FA. Laparoscopic hepaticojejunostomy for the treatment of bile duct injuries in difficult scenarios (with video). Mini-invasive Surg 2022;6:47. http://dx.doi.org/10.20517/2574-1225.2022.50
AMA Style
Pinsak A, Gielis M, Viscido G, Doniquian AM, Alvarez FA. Laparoscopic hepaticojejunostomy for the treatment of bile duct injuries in difficult scenarios (with video). Mini-invasive Surgery. 2022; 6: 47. http://dx.doi.org/10.20517/2574-1225.2022.50
Chicago/Turabian Style
Pinsak, Agustin, Manuel Gielis, Germán Viscido, Alejandro M. Doniquian, Fernando A. Alvarez. 2022. "Laparoscopic hepaticojejunostomy for the treatment of bile duct injuries in difficult scenarios (with video)" Mini-invasive Surgery. 6: 47. http://dx.doi.org/10.20517/2574-1225.2022.50
ACS Style
Pinsak, A.; Gielis M.; Viscido G.; Doniquian AM.; Alvarez FA. Laparoscopic hepaticojejunostomy for the treatment of bile duct injuries in difficult scenarios (with video). Mini-invasive. Surg. 2022, 6, 47. http://dx.doi.org/10.20517/2574-1225.2022.50
About This Article
Copyright
Data & Comments
Data
 Cite This Article 9 clicks
Cite This Article 9 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.