Impact of intrapartum antibiotics on the developing microbiota: a review
Abstract
The perinatal period sets the basis for the later physiological and immune homeostasis of the individual, with the intestinal microbiota being an important contributor to driving this homeostasis development. Therefore, the initial establishment and later development of the microbiota during early life may play a key role in later health. This early establishment of the intestinal microbiota is known to be affected by several factors, with gestational age, delivery mode, and feeding habits being extensively studied ones. Other factors are not so well understood, although knowledge has been accumulating in the last years. Among them, a factor of great relevance is the effect of perinatal exposure to antibiotics. Administration of intrapartum antimicrobial prophylaxis (IAP) to women during the delivery process represents the most common form of exposure to antibiotics during the perinatal period, present in around 30% of deliveries. During the last decade, evidence has accumulated demonstrating that IAP alters intestinal microbiota development in neonates. Moreover, recent evidence indicates that this practice may also be altering the infant intestinal resistome by increasing the levels of some antibiotic resistance genes. This evidence, as reviewed in this manuscript, suggests the interest in promoting the rational use of IAP. This practice has significantly reduced the risk of neonatal infections, but now the accumulating knowledge suggests the need for strategies to minimize its impact on the neonatal microbiota establishment.
Keywords
INTRODUCTION
The microbial colonization of the infant gut during the perinatal period is critical for the later health of the baby since the interplay of the microbiota with the host is a major force for the proper development of the homeostatic systems[1]. Thus, early colonization is key for later health, constituting a “window of opportunity” for microbiota modulation towards a healthy composition with long-term beneficial effects, as suggested by the “microbiota hypothesis”[2].
Initially, the process starts with the settlement of facultative anaerobes, such as enterobacteria, and aerotolerant microorganisms. These microbes reduce the oxygen level in the gut environment allowing the multiplication of strict anaerobes, such as Bifidobacterium or Bacteroides, later followed by the increase of different clostridia members until, at the age of three years, the microbiota reaches a composition close to that found in adults, although not totally the same[3].
This initial colonization of the infant is highly dependent on different factors, with gestational age at delivery, mode of delivery, and infant feeding habits being the most extensively studied ones[4,5]. Another factor also known to influence this early colonization process is exposure to perinatal antibiotics. The most common form of exposure to antibiotics at the perinatal stage is intrapartum antimicrobial prophylaxis (IAP)[6,7].
Some decades ago, group B streptococci (GBS) was the neonatal pathogen showing higher morbidity and mortality, with mortality rates reaching 50% of infected babies. Then, in the 1980s, it was evidenced that administration of antibiotics to the mother during delivery was efficacious for preventing neonatal GBS infection. Therefore, recommendations on the use of IAP to reduce the risk for maternal-filial transfer of GBS were issued since this pathogen was common, being present in approximately 10%-30% of women[8]. This has been a successful approach, with the cases of GBS infection dropping about ten times since then[8,9]. The decision on whether and how to administer IAP to mothers is managed in different ways in different countries; some perform a prenatal screening for GBS carriage and only treat the positive mothers with IAP, whereas other countries use risk factor (prolonged rupture of membranes, intrapartum fever, etc.) assessment to decide on whether to administer IAP. Most often, IAP consists of the intravenous administration of penicillin or, alternatively, ampicillin. During the last years, the identification of the potential ability of IAP to induce alterations in the gut colonization process, together with interest in reducing antibiotic use, have attracted attention to the study of the impact of this prophylaxis. This is especially relevant since IAP is present in more than 30% of total vaginal deliveries[6]. Moreover, IAP is also common due to C-section practices, being recommended in all C-section deliveries since it reduces by more than half the complications of this surgery[10]. In this case, the antibiotic most commonly administered is cefazolin, except in the case of allergy[11].
The present review summarizes the current works in the gut microbiota field, analyzing IAP as an impact factor on its composition and function as well as the antibiotic resistance gene (ARG) load. A comprehensive search was conducted in the PubMed database. The search strategy combined the terms “gut microbiota”, “intestinal microbiota”, “neonate”, “infant”, “intrapartum antimicrobial prophylaxis”, “IAP”, “intrapartum antibiotics”, “delivery”, “group B streptococci”, “GBS”, “resistome”, and “antibiotic resistance genes”. References from included studies matching the inclusion terms, but not found with the search strategy used, were also included. Searches were limited to studies on humans, written in English, and published papers. No offspring age limit or date of publication restriction was used. The following data were extracted: year of study publication, country, characteristics of study population such as sample size (IAP group and control group, if it existed), delivery mode, gestational age at birth, antibiotic administration at delivery, time-point of stool collection, microbiota analyses methodology, gut microbiota composition, and resistome results.
IMPACT OF IAP ON THE DEVELOPING MICROBIOTA COMPOSITION
Antibiotics are one of the main factors affecting the correct gut microbiota development and stability[12]. Different studies have focused on the effect of antibiotics directly administered to the individual; however, until recently, data on how antibiotics administered to mothers during delivery could affect the early microbiome colonization of the infant were scarce. In 2004, the first paper comparing the colonization patterns of gut microbiota in neonates born to mothers with and without amoxicillin for GBS prophylaxis was published[13]. This study found that only Clostridium, of the six bacterial groups analyzed by stool culturing, showed statistical differences among the groups, with lower counts in the IAP group of babies. No differences in other groups, such as Bifidobacterium, Bacteroides, or enterobacteria, were observed in this culture-based study. The topic was then forgotten until 2014, when Aloisio et al. published a paper using qPCR, a culture-independent technique[14]. They observed a negative impact of ampicillin for GBS prophylaxis in genus Bifidobacterium in seven-day-old infants’ feces, but the other bacterial groups analyzed were not significantly affected by the maternal treatment. It was not until 2015 that when a study using massive sequencing techniques of the 16S rRNA gene became available, reporting the effect of IAP upon the microbiota in a study with neonates born prematurely[15]. The authors found that the impact of IAP on the developing gut microbiota was even higher than the effect of direct administration of antibiotics to babies during the first days of life. Since then, more than 20 papers specifically examining the relationship between the IAP and gut microbiome have been published.
In the observational cohort of very low birth weight babies study conducted by Arboleya et al., the direct administration of antibiotics to infants during the first days of life and/or to mothers during labor were compared[15]. The results show that, at one month of age, babies from IAP mothers and without other antibiotic exposure harbored lower relative abundances of different bacterial families, such as Bifidobacteriaceae, Streptococacceae, and Staphylococcaceae, and higher percentages of Enterobacteriaceae; these data were further confirmed by qPCR analyses. The comparison with cases where the baby has received antibiotics directly, not via IAP, indicated that IAP had an equal or even higher negative effect on the microbiota establishment in the infant. Later studies conducted with the same infant cohort showed that babies from mothers who had received IAP harbor lower abundances of Actinobacteria, higher levels of Firmicutes and Proteobacteria, and lower levels of acetate and total short-chain fatty acids in their gut microbiota[16]. Moreover, the study concluded that IAP may involve lasting effects on physiology, which could affect the neonatal microbiota-host crosstalk with long-lasting effects on health, due to the observed differences in inferred metabolic pathways affected by the IAP treatment. Similarly, in a study comparing the gut microbiota composition in meconium of a cohort of prematurely born babies with and without IAP and the vaginal microbiota of mothers, Zhou et al. observed that the Lactobacillus population was decreased after IAP in the mothers’ vagina and newborns’ meconium samples[17]. In addition, they observed specific alterations in meconium (Staphyloccous or Sphingomonas increment) from some IAP premature babies diagnosed with early-onset sepsis (EOS). This may indicate an association between EOS and antibiotic-mediated dysbiosis in the premature gut.
It is important to take into consideration that prematurely born babies are a cohort of neonates very exposed to medications and clinical practices due to their underdevelopment at birth. Thus, the gut microbiota establishment in those babies is a challenging process due to different factors surrounding organ immaturity, long stays at hospitals, medications, oxygen support, antibiotics, etc., and, therefore, they may not be very representative of the situation in healthy full-term infants. For this reason, most of the studies focused on the effect of IAP on gut microbiota development have been performed in full-term infants since these represent a more common situation. Moreover, in most cases, the studies used vaginally delivered babies, although some studies have also included infants born by C-section [Table 1], in most cases observing different findings depending on delivery mode. One of the first studies published with full-term neonates was carried out in a cohort of Canadian babies, where the effect on the intestinal microbiota composition of penicillin (in vaginal deliveries) and cefazolin (in emergency and elective C-sections) were studied at three months of age[18]. Changes in the gut microbiota were observed, with depletion of Bacteroidetes and loss of diversity among the most significant results. Moreover, the relative abundances of Bacteroides and Parabacteroides genera were decreased, while Enterococcus, Clostridium, and Proteobacteria were increased after IAP in the three groups of babies analyzed[18].
Main demographic and technical characteristics of studies investigating the effect of IAP on gut microbiota development included in this review
| Study population (delivery mode/n [n in IPA group]/stool collection age) | Antibiotic | Technique for gut microbiota analyses | Refs. |
| Full-term, vaginal and C-section/n = 50 [n = 23 and | Amoxicillin | Culturing stool samples | [13] |
| Full-term, vaginal/n = 52 [n = 26]/7 days | Ampicillin | qPCR, PCR-DGEE | [14] |
| Very low birth-weight preterm (24-32 GW)/n = 27 | Penicillin (n = 1), ampicillin (n = 1), or ampicillin + erythromycin (n = 12) | 16S rRNA amplicon sequencing (V3, Ion Torrent), qPCR | [15, 16] |
| Full-term and preterm (< 37 GW) (vaginal and C-section)/n = 50 and 48 [n = 27 and n = 25]/meconium | Cefazolin | 16S rRNA amplicon sequencing (V4, Illumina) | [17] |
| Full-term vaginal and C-Section/n = 189 [n = 42 and n = 43]/3, 12 months | Penicillin (vaginal), cefazolin (C-section) | 16S rRNA amplicon sequencing (V4, Illumina) | [18] |
| Full-term, vaginal/n = 40 [n = 18]/2, 10, 30, 90 days | Penicillin | 16S rRNA amplicon sequencing (V3, Illumina) | [19] |
| Full-term, vaginal/n = 149 [n = 44]/0, 1, 2, 3, 4 days, 6 months | Penicillin (n = 38), cefuroxime (n = 4), clindamycin (n = 2) | 16S rRNA amplicon sequencing (V4-5, Ion Torrent), shotgun metagenomics (Illumina) | [20] |
| Full-term, vaginal and C-section/n = 74 [n = 14 and | Penicillin (vaginal); cefazolin (n = 5), ampicillin (n = 1) and penicillin (n = 1) | 16S rRNA amplicon sequencing (V3, Illumina) | [21] |
| Full-term, vaginal and C-section/n = 130 [n = 14]/1, 3, 6 months | Ampicillin (vaginal), cefazolin (C-section) | 16S rRNA amplicon sequencing (V3-V4, Illumina) | [22] |
| Full-term, vaginal/n = 100 [n = 27]/12 months | Penicillin (n = 25), cefuroxime (n = 2), | 16S rRNA amplicon sequencing | [23] |
| Full-term, vaginal/n = 266 [n = 87]/6 weeks, 12 months | Penicillin (n = 55), | 16S rRNA amplicon sequencing (V4-V5, Illumina) | [24] |
| Full-term, vaginal/n = 26 [n = 13]/7, 30 days | Ampicillin | 16S rRNA amplicon sequencing (V3-V4, Illumina), qPCR | [25] |
| Full-term vaginal and C-Section/n = 1654 [n = 375 and n = 403]/3 months | Penicillin (vaginal), cefazolin (C-section) | 16S rRNA amplicon sequencing (V4, Illumina), qPCR | [26] |
| Elective C-Section/n = 44 [n = 44]/10 days, 9 months | Cefuroxime | 16S rRNA amplicon sequencing (V3-V4, Illumina) | [27] |
| Full-term C-Section and vaginal/n = 63 [n = 40 and | Cefuroxime (C-section) | 16S rRNA amplicon sequencing (V3-V4 first month, V4 3 years - Illumina), shotgun metagenomics (7, 28 days - Illumina) | [28] |
| Full-term, vaginal/n = 84 [n = 35]/7, 30 days | Ampicillin | qPCR | [29] |
| Full-term, vaginal and C-section/n = 43 [n = 7 and | Ampicillin (vaginal), cefazolin (C-section) | ITS (16S-23S) amplicon sequencing (Illumina), qPCR | [30] |
The vast majority of studies focusing on full-term vaginally delivered babies showed important changes in the gut microbiota composition during the first months of life, with a lower number of studies with follow-up at later ages. Some alterations in the intestinal microbiota were also detected during the first days of life by different authors. In meconium samples of both premature and full-term babies from IAP mothers, lower levels of lactobacilli were observed[17]. At seven days of life, after penicillin prophylaxis during delivery, lower diversity and lower abundance of Bifidobacteriaceae (and significantly lower in genus Bifidobacterium), Bacteroidaceae, Lachnospiraceae, or Lactobacillaceae were observed, followed by enrichment in Enterobacteriaceae, Clostridiaceae, or Streptococcaceae in an Italian cohort of babies subjected to 16S rRNA gene sequencing[14]. Some of these observations were corroborated by Nogacka et al. in a Spanish cohort of vaginally delivered full-term babies at 10 days of age[19]. They showed higher proportions of Proteobacteria, Clostridiaceae, and S24-7 families in an IAP group of neonates and lower abundances of Bifidobacteriaceae. In agreement with these data, Bacteroides was also one bacterial group decreased while Proteobacteria and Clostridium increased during the first days of life in a group of four-day-old IAP babies from Finland[20].
At one and three months of age, Nogacka et al. still continued detecting differences due to IAP treatment, with significant enrichment of Campylobacteriaceae, Helicobacteraceae, Prevotellaceae, and S24-7 families and lower levels of alpha-diversity, in general and specifically of Bifidobacteriaceae, in IAP babies[19]. Similar results were found by Stearns et al. in a Canadian cohort of vaginal full-term infants at six and twelve weeks, where lower microbial diversity and bifidobacterial abundances were observed, in addition to an increment of Clostridium and Escherichia genera[21]. A low abundance of Bifidobacterium was also detected in Japanese infants whose mothers were administered intrapartum antibiotics in both vaginal (ampicillin) and C-section (cefazolin) delivery[22].
An examination of the impact of IAP on the gut microbiota beyond the third month of life has been conducted in a few cohorts of babies. While Imoto et al.[22] did not observe any statistical differences in a group of six-month-old infants, Tapianien et al.[20] pointed out that the effect of IAP could be comparable with that caused by direct postnatal antibiotics, with lower levels of Bacteroides still being present at six months of age. This cohort of babies was also examined at one year of age, and the authors found consistent results, with lower relative abundances of Bacteroidetes and Bacteroides and an increase of Escherichia coli in the IAP group[23]. Similarly, Azad et al. also observed alteration in the gut microbiota at one year of age in their Canadian cohort[18]. These were mainly characterized by higher relative abundances of Clostridiaceae in the vaginally delivered IAP group as well as in an IAP emergency C-section group where, in addition, lower diversity and proportions of Bacteroides were observed.
In 2020, a prospective study was carried out to evaluate the impact of the different specific classes of antibiotics administered as IAP. Lower abundance of Bacteroides, Bifidobacterium Ruminococcus, Blautia, and Roseburia and higher proportions of Oscillospora and Veillonella were found at both six weeks and one year of age after the exposure to any class of antibiotics[24]. In addition, the authors concluded that IAP alters the natural development and trajectory of the infant gut microbiome; its effects persist after one year of life, and particular alterations were associated with specific antibiotics. Over time, they observed a smaller increase in Bacteroides and Bifidobacterium and a rise in Coprococcus in infants exposed to penicillin. Cephalosporin entailed a smaller increment in Bifidobacterium and Enterococcus, and when a mix of antibiotics was used, a decrease in E. coli abundance was observed, in comparison with a non-IAP group of neonates. Moreover, differentially abundant functional metagenomes were also observed at one year of age[24].
Breastfeeding is one of the most influential factors impacting gut microbiome development, and it is usually a confounder when the impact of other perinatal factors is questioned. Some of the studies focusing on IAP impact also examined the impact of breastfeeding on gut microbiota acquisition after perinatal antibiotics. Mazzola et al. studied the impact of IAP in breastfed and formula-fed infants and observed a different evolution of the gut microbiota during the first month of life[25]. IAP breastfed infants showed lower diversity and absence of Bifidobacterium at seven days and recovery at one month, but with a dominance of enterobacteria in their gut microbiota. However, IAP formula-fed infants showed a dominance of Bacteroidetes at one month, with respect to no IAP formula-fed and IAP breastfed infants. Nogacka et al. also suggested a differential response to IAP treatment depending on the feeding mode[19]. Azad et al. suggested a protective role of breastfeeding in babies exposed to IAP due to emergency C-sections and breastfed at least for three months[18]. However, in an extended Canadian cohort of babies[26], the authors observed significantly lower proportions of Bifidobacterium in exclusively or partially breastfed, vaginally delivered IAP-treated infants. Those inconsistent findings reported by different studies indicate the need for more studies on the role of breastfeeding as a modulator of the IAP-induced alterations in the infant microbiota development process.
As stated above, few studies have focused specifically on the impact of IAP in C-section delivered babies. Apart from the information unveiled by Azad et al.[18] with respect to the changes observed after IAP in emergency and elective C-sections, in the same year, Stearns et al.[21] also included a group of C-section babies in their study. The authors concluded that IAP has an impact independent of delivery type in the gut microbiota development during the first three months of life, with a special negative impact on Bacteroidetes. Chen et al. also observed a severe depletion of Bacteroidetes and an increment in Firmicutes and Proteobacteria in C-section delivery after maternal IAP exposure[26]. Other studies aimed at unraveling the effect of IAP timing on C-sections have concluded that C-section delivery affects the gut microbiome colonization more strongly than antenatal antibiotic exposure[27,28]. These studies did not observe differences between the group of babies whose mothers received antibiotics prior to skin incision or those after umbilical cord clamping, with Bacteroides and Bifidobacterium most negatively affected and Proteobacteria increased at one month of life, but not at three years of age, with respect to a control group of vaginal-delivery babies[28].
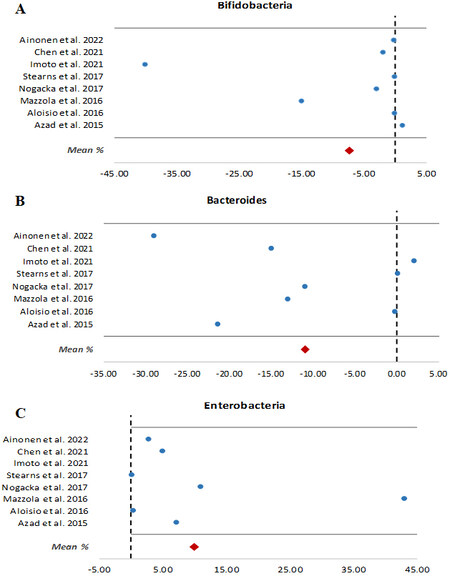
Most of the studies revealed that Bifidobacterium and Bacteroides are two of the taxa more vulnerable to maternal prophylactic antibiotics, although Imoto et al. found that a reduction in Bacteroides was more associated with C-section delivery than with IAP treatment[22]. It was observed that IAP reduced not only the relative abundances of genus Bifidobacterium but also its absolute quantities, as was confirmed by qPCR[14,15,29]. Moreover, not only at the genus level but also at the species level, the negative impact of IAP has been demonstrated on bifidobacteria populations by DGGE-PCR[14] and ITS-sequencing[30]. A 7.2% relative abundance decrement of this genus per each hour of IAP against GBS in vaginal births was also observed by Stearns et al.[21]. Conversely, most studies showed that, in this dysbiosis situation, Proteobacteria increase in abundance. Figure 1, encompassing eight studies with relative abundances available in their respective manuscripts for bifidobacteria, bacteroides, and enterobacteria at genus or family level, shows how the two former taxa are negatively affected by IAP, while enterobacteria are increased in the gut microbiota of full-term vaginally delivered babies at 7-90 days old.
Figure 1. Changes in the relative abundances (%) as a result of IAP exposure in different studies of: (A) bifidobacteria; (B) bacteroides; and (C) enterobacteria. Data are from between 7 and 90 days of life, with the exception of the Ainonen et al.’s study[23], which was conducted at one year in full-term vaginally delivery babies. Mean (%) was calculated from the relative abundances numerically available in the eight studies included. IAP: Intrapartum antimicrobial prophylaxis.
Long-term effects of IAP on the gut microbiota, further than those reported at one year of age, have not been published yet. However, a higher risk of cerebral palsy or bowel dysfunctions in children who were born prematurely and whose mothers were administered erythromycin were observed at the age of seven years[31], while a relationship between IAP for GBS prophylaxis and BMI-Z scores was not detected in children at 2-5 years[32]. Beyond gut microbiota, some studies have also been published showing differences in the infant oral microbiota due to maternal intrapartum antibiotics[33,34].
IMPACT OF IAP ON THE DEVELOPING INFANT RESISTOME
As discussed above, different authors showed how IAP affects the initial establishment of the infant gut microbiota and how different bacterial groups vary as a function of this perinatal factor. However, little is known about the connection between IAP and the infant gut resistome since few authors have thus far looked into this matter.
Nogacka et al. assessed the prevalence of 11 ARGs in one-month-old infants born at term by vaginal delivery[19]. The prevalence of the ARGs blaTEM, CTX-M, and aac6-aph2 was higher in the group of children whose mothers received prophylaxis. Among these three genes, blaTEM was present in 20% more infants in the IAP group than in the control group. A recent study suggested a potential detrimental impact of IAP on increasing the risk for harboring ARGs at one year of age, although delivery mode (C-section) was found to be an important confounding factor in infant resistome studies[35]. Tapiainen et al. studied not only the effect of IAP but also the direct administration of antibiotics to the newborn after birth and the resulting combination of both factors on infant gut microbiota[20]. Although their data in the resistome should be taken with caution, as the number of samples was low and the infants received a probiotic, the results show that this group of infants harbor an increased abundance of ARGs in their gut microbiota. The most commonly detected ARGs were related to the presence of species belonging to the genera Escherichia and Staphylococcus. They also analyzed the presence of ARGs in the gut microbiota of the mothers and found that they had a lower burden of ARGs compared to their offspring. The same cohort in Tapiainen’s study was also used by Li et al. to test whether these genes were vertically transmitted from mothers to infants[36]. Metagenomics analyses allowed them to identify the origin of the species carrying the resistance genes present in children’s feces by comparing mother and infant samples. The results show that vertical transmission decreased with the administration of antibiotics to both the mother and the newborn. The altered gut colonization caused by antibiotics led to the establishment of bacteria from the environment rather than from the mother’s microbiota. In this study, the resistance genes of most of the children in the antibiotic group came from species found in the hospital environment. In contrast, in the control group, the species carrying the genes were also found in the maternal gut microbiota.
In other works, ARG burden was directly related to the presence of certain bacteria, which could entail a direct risk to infants’ health, since the association of IAP with an increased presence of antibiotic-resistant bacteria in the intestinal microbiota of newborns, predisposing to late-onset bacterial infections, has been reported[37,38]. In fact, the use of IAP has been associated with an increase in GBS resistance to antibiotics such as clindamycin and erythromycin[9]. Along the same line, Pärnänen et al. determined that IAP increased the presence of ARGs and mobile genetic elements in the infant gut microbiota[39]. They associated a higher load of ARGs with higher counts of E. coli and different species of gamma-proteobacteria and with a decreased presence of bifidobacteria. Conversely, IAP has also been associated with increased ARGs not only in the gut but in other parts of the organism, such as the nasopharynx[40]. This study found that infants born to mothers treated with azithromycin had a higher prevalence of the msrA and ermC genes, which confer macrolide resistance, at 28 days of age. These genes were positively associated with the presence of AZI-resistant Staphylococcus aureus. Moreover, other authors have also reported a higher prevalence of
Despite the different methodologies used, most authors agree that IAP alters the initial establishment of the intestinal microbiota, which may predispose infants to various pathologies and infections. This alteration, together with the selective pressure exerted by antibiotics, favors the presence of bacteria carrying antibiotic resistance genes.
DISCUSSION
The data accumulated during the last decade clearly demonstrate that the use of IAP alters the early-life microbial colonization process, affecting the intestinal microbiota composition during these very important early days of life. Although some differences in the effects reported by different authors do exist, there are also some common and reproducible observations. These include the increased levels of enterobacteria and reduction of strict anaerobe commensals such as bifidobactera and bacteroides during the first months of life. The long-term persistence of these differences is a current matter of debate since few studies have addressed this aspect and the techniques more frequently used, mainly 16S rRNA gene profiling and qPCR, allow for a general microbiota composition overview but do not provide data on potential strain replacements and other effects at the strain level. Similarly, our understanding of the long-term effects on the health of these early IAP-induced microbiota alterations is still very limited.
Moreover, recent evidence also suggests a potential detrimental effect of IAP on the infant intestinal resistome. Although only few studies on this subject have been published to date, those available suggest an impact. In a context with increasing problems due to antimicrobials-resistant microorganisms, and given the potential role of the gut microbiota as a reservoir for ARGs, understanding the effects of early-life interventions on the ARG pool and level is of great interest. Metagenomic studies, allowing for resistome analyses, are becoming available in this area, and they will provide new insight into this aspect.
To conclude, the evidence underlined in this manuscript, together with the demonstrated efficacy of IAP for avoiding GBS infections in the neonate, points to the need for rational use of IAP. This highlights the importance of intervention strategies limiting the impact of IAP on the infant gut microbiota composition and resistome, and the resulting long-term health implications.
DECLARATIONS
Authors’ contributionsMade substantial contributions to conception and design of the study, reviewed the literature and performed data analysis and interpretation: Arboleya S, Saturio S, Gueimonde M
Availability of data and materialsNot applicable.
Financial support and sponsorshipThis work was supported by Grant name AGL2017-83653R funded by the Spanish “Ministerio de Ciencia, Innovación y Universidades (MCIU), Agencia Estatal de Investigación (AEI) and FEDER”. Arboleya S was the recipient of a Juan de la Cierva Postdoctoral Contract (Ministry of Science, Innovation and Universities, MCIN/AEI/10.13039/501100011033, Ref. IJCI-2017-32156) and Saturio S is the recipient of a predoctoral contract from ISPA.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Sommer F, Bäckhed F. The gut microbiota - masters of host development and physiology. Nat Rev Microbiol 2013;11:227-38.
2. Rautava S, Ruuskanen O, Ouwehand A, Salminen S, Isolauri E. The hygiene hypothesis of atopic disease - an extended version. J Pediatr Gastroenterol Nutr 2004;38:378-88.
3. Milani C, Duranti S, Bottacini F, et al. The first microbial colonizers of the human gut: composition, activities, and health implications of the infant gut microbiota. Microbiol Mol Biol Rev 2017;81:e00036-17.
4. Arrieta MC, Stiemsma LT, Amenyogbe N, Brown EM, Finlay B. The intestinal microbiome in early life: health and disease. Front Immunol 2014;5:427.
5. Bäckhed F, Roswall J, Peng Y, et al. Dynamics and stabilization of the human gut microbiome during the first year of life. Cell Host Microbe 2015;17:690-703.
6. Van Dyke MK, Phares CR, Lynfield R, et al. Evaluation of universal antenatal screening for group B Streptococcus. N Engl J Med 2009;360:2626-36.
7. Chai G, Governale L, McMahon AW, Trinidad JP, Staffa J, Murphy D. Trends of outpatient prescription drug utilization in US children, 2002-2010. Pediatrics 2012;130:23-31.
8. Di Renzo GC, Melin P, Berardi A, et al. Intrapartum GBS screening and antibiotic prophylaxis: a European consensus conference. J Matern Fetal Neonatal Med 2015;28:766-82.
9. Verani JR, McGee L, Schrag SJ. Division of Bacterial Diseases; National Center for Immunization and Respiratory Diseases; Centers for Disease Control and Prevention. Prevention of perinatal group B Streptococcal disease - revised guidelines from CDC, 2010. MMWR Recomm Rep 2010;59:1-36.
10. Smaill FM, Grivell RM. Antibiotic prophylaxis versus no prophylaxis for preventing infection after cesarean section. Cochrane Database Syst Rev 2014;2014:CD007482.
11. Eley VA, Christensen R, Ryan R, et al. Prophylactic cefazolin dosing in women with body mass index > 35 kg·m-2 undergoing cesarean delivery: a pharmacokinetic study of plasma and interstitial fluid. Anesth Analg 2020;131:199-207.
12. Ianiro G, Tilg H, Gasbarrini A. Antibiotics as deep modulators of gut microbiota: between good and evil. Gut 2016;65:1906-15.
13. Jauréguy F, Carton M, Panel P, Foucaud P, Butel MJ, Doucet-Populaire F. Effects of intrapartum penicillin prophylaxis on intestinal bacterial colonization in infants. J Clin Microbiol 2004;42:5184-8.
14. Aloisio I, Mazzola G, Corvaglia LT, et al. Influence of intrapartum antibiotic prophylaxis against group B Streptococcus on the early newborn gut composition and evaluation of the anti-Streptococcus activity of Bifidobacterium strains. Appl Microbiol Biotechnol 2014;98:6051-60.
15. Arboleya S, Sánchez B, Milani C, et al. Intestinal microbiota development in preterm neonates and effect of perinatal antibiotics. J Pediatr 2015;166:538-44.
16. Arboleya S, Sánchez B, Solís G, et al. Impact of prematurity and perinatal antibiotics on the developing intestinal microbiota: a functional inference study. Int J Mol Sci 2016;17:649.
17. Zhou P, Zhou Y, Liu B, et al. Perinatal antibiotic exposure affects the transmission between maternal and neonatal microbiota and is associated with early-onset sepsis. mSphere 2020;5:e00984-19.
18. Azad MB, Konya T, Persaud RR, et al. CHILD Study Investigators. Impact of maternal intrapartum antibiotics, method of birth and breastfeeding on gut microbiota during the first year of life: a prospective cohort study. BJOG 2016;123:983-93.
19. Nogacka A, Salazar N, Suárez M, et al. Impact of intrapartum antimicrobial prophylaxis upon the intestinal microbiota and the prevalence of antibiotic resistance genes in vaginally delivered full-term neonates. Microbiome 2017;5:93.
20. Tapiainen T, Koivusaari P, Brinkac L, et al. Impact of intrapartum and postnatal antibiotics on the gut microbiome and emergence of antimicrobial resistance in infants. Sci Rep 2019;9:10635.
21. Stearns JC, Simioni J, Gunn E, et al. Intrapartum antibiotics for GBS prophylaxis alter colonization patterns in the early infant gut microbiome of low risk infants. Sci Rep 2017;7:16527.
22. Imoto N, Kano C, Aoyagi Y, et al. Administration of β-lactam antibiotics and delivery method correlate with intestinal abundances of Bifidobacteria and Bacteroides in early infancy, in Japan. Sci Rep 2021;11:6231.
23. Ainonen S, Tejesvi MV, Mahmud MR, et al. Antibiotics at birth and later antibiotic courses: effects on gut microbiota. Pediatr Res 2022;91:154-62.
24. Coker MO, Hoen AG, Dade E, et al. Specific class of intrapartum antibiotics relates to maturation of the infant gut microbiota: a prospective cohort study. BJOG 2020;127:217-27.
25. Mazzola G, Murphy K, Ross RP, et al. Early gut microbiota perturbations following intrapartum antibiotic prophylaxis to prevent group B Streptococcal disease. PLoS One 2016;11:e0157527.
26. Chen YY, Zhao X, Moeder W, et al. Impact of maternal intrapartum antibiotics, and caesarean section with and without labour on Bifidobacterium and other infant gut microbiota. Microorganisms 2021;9:1847.
27. Kamal SS, Hyldig N, Krych Ł, et al. Impact of early exposure to cefuroxime on the composition of the gut microbiota in infants following cesarean delivery. J Pediatr 2019;210:99-105.e2.
28. Dierikx T, Berkhout D, Eck A, et al. Influence of timing of maternal antibiotic administration during caesarean section on infant microbial colonisation: a randomised controlled trial. Gut 2021; doi: 10.1136/gutjnl-2021-324767.
29. Corvaglia L, Tonti G, Martini S, et al. Influence of intrapartum antibiotic prophylaxis for group B Streptococcus on gut microbiota in the first month of life. J Pediatr Gastroenterol Nutr 2016;62:304-8.
30. Saturio S, Suárez M, Mancabelli L, et al. Effect of intrapartum antibiotics prophylaxis on the bifidobacterial establishment within the neonatal gut. Microorganisms 2021;9:1867.
31. Kenyon S, Pike K, Jones D, et al. Childhood outcomes after prescription of antibiotics to pregnant women with spontaneous preterm labour: 7-year follow-up of the ORACLE II trial. The Lancet 2008;372:1319-27.
32. Metz TD, McKinney J, Allshouse AA, Knierim SD, Carey JC, Heyborne KD. Exposure to group B Streptococcal antibiotic prophylaxis and early childhood body mass index in a vaginal birth cohort. J Matern Fetal Neonatal Med 2020;33:3318-23.
33. Gomez-Arango LF, Barrett HL, McIntyre HD, Callaway LK, Morrison M, Dekker Nitert M. Antibiotic treatment at delivery shapes the initial oral microbiome in neonates. Sci Rep 2017;7:43481.
34. Li M, Shi B, Ma J, Peng X, Shi J. Comparing prophylactic use of cefazolin for SSI in cesarean section: a systematic review and meta-analysis. Arch Gynecol Obstet 2021;303:313-20.
35. Lebeaux RM, Coker MO, Dade EF, et al. The infant gut resistome is associated with E. coli and early-life exposures. BMC Microbiol 2021;21:201.
36. Li W, Tapiainen T, Brinkac L, et al. Vertical transmission of gut microbiome and antimicrobial resistance genes in infants exposed to antibiotics at birth. J Infect Dis 2021;224:1236-46.
37. Glasgow TS, Young PC, Wallin J, et al. Association of intrapartum antibiotic exposure and late-onset serious bacterial infections in infants. Pediatrics 2005;116:696-702.
38. Ashkenazi-Hoffnung L, Melamed N, Ben-Haroush A, Livni G, Amir J, Bilavsky E. The association of intrapartum antibiotic exposure with the incidence and antibiotic resistance of infantile late-onset serious bacterial infections. Clin Pediatr (Phila) 2011;50:827-33.
39. Pärnänen K, Karkman A, Hultman J, et al. Maternal gut and breast milk microbiota affect infant gut antibiotic resistome and mobile genetic elements. Nat Commun 2018;9:3891.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Arboleya S, Saturio S, Gueimonde M. Impact of intrapartum antibiotics on the developing microbiota: a review. Microbiome Res Rep 2022;1:22. http://dx.doi.org/10.20517/mrr.2022.04
AMA Style
Arboleya S, Saturio S, Gueimonde M. Impact of intrapartum antibiotics on the developing microbiota: a review. Microbiome Research Reports. 2022; 1(4): 22. http://dx.doi.org/10.20517/mrr.2022.04
Chicago/Turabian Style
Arboleya, Silvia, Silvia Saturio, Miguel Gueimonde. 2022. "Impact of intrapartum antibiotics on the developing microbiota: a review" Microbiome Research Reports. 1, no.4: 22. http://dx.doi.org/10.20517/mrr.2022.04
ACS Style
Arboleya, S.; Saturio S.; Gueimonde M. Impact of intrapartum antibiotics on the developing microbiota: a review. Microbiome. Res. Rep. 2022, 1, 22. http://dx.doi.org/10.20517/mrr.2022.04
About This Article
Copyright
Data & Comments
Data
 Cite This Article 13 clicks
Cite This Article 13 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.