State of evidence and future perspectives in minimally invasive management of gastroesophageal reflux disease (GERD)
Abstract
The future of minimally invasive treatment of gastroesophageal reflux disease (GERD) will be realized through collaborative precision medicine more than any foreseeable new technology. Multidisciplinary foregut societies are fostering the collaboration and expertise needed to provide a personalized treatment of GERD. Patient-centric therapy will consider combination therapies’ clinical successes. Taking a patient uncontrolled on medication to controlled via a combination of medicine and a procedure will replace the historical mutual exclusivity of acid-suppressive medication or surgery as a treatment for GERD. Research directed at precision medicine will focus on subgroup analysis rather than randomized controlled trials. Recognition of the crural diaphragm as a reflux barrier which fails in GERD patients regardless of the presence of an axial hernia has resulted from modalities such as 3-D high-resolution impedance manometry, endoscopic ultrasound, functional luminal impedance planimetry. More precise patient selection for purely endoscopic therapies will be possible.The concept of hernia reduction will be replaced by calibration of the crural repair to restore its sphincteric function. Partnering a surgically calibrated hernia repair partnered with interventional gastrointestinal endoscopic reinforcement of the lower esophageal sphincter will foster physician alliances and offer patient-centric alternatives to traditional fundoplication. As such, laparoscopic Nissen Fundoplication will lose its historical primacy and be relegated to the most severe GERD. Magnetic sphincter augmentation (LINX®), varing degrees of partial fundoplication, and endoluminal therapies with or without hiatal hernia repair will become the mainstay of GERD AntiReflux Procedures. Radio Frequency modulation (Stretta®) may be an alternative to neuromodulators in treating the acid-sensitive esophagus. The nascent era of endoscopic robotics will improve precision, reproducibility and revive natural orifice transluminal endoscopic surgery.
Keywords
INTRODUCTION
Future developments in minimally invasive management of gastroesophageal reflux disease (GERD) will stem more from multidisciplinary collaboration leading to individualized, expert care than from novel technologies. Open discussion and consensus-building are replacing a historical enmity between surgeons (who regarded acid-suppressive medications (ASMs) as bad and thought patients were underserved by surgery) and gastroenterologists (who recognized the success of ASMs and dealt with train wrecks from improperly performed surgery).
Newly formed multidisciplinary societies such as the American Foregut Society (AFS) and the European Foregut Society have promoted collaboration and consensus-building between gastroenterologists and foregut surgeons. Within the AFS, the committees, meetings, educational programs, and social media are co-chaired by surgical and medical specialists. An expert-moderated forum for case presentation discussion, DocMatter, has similarly allowed gastroenterologists and surgeons to weigh-in on patient-centric care. AFS’s journal Foregut completed its first year of publication in 2021 and is co-edited by both surgeons and gastroenterologists from the United States and Europe. These efforts are moving the bar towards specialization and patient-centric precision medicine.
The preceding articles in this issue highlight the need for and presence of minimally invasive antireflux procedures (ARPs) to address the needs of patients with incomplete control of GERD yet unwilling to undergo a laparoscopic Nissen fundoplication. Research using precision medicine principles is needed to properly select which patients will benefit most from these varied ARPs.
GERD is not one disease; it encompasses a spectrum from reflux burden to perceptive response [Figure 1]. Reduced quality of life stems from anatomic, physiologic, and cognitive factors, which often overlap in the same patient. Addressing all of the appropriate elements in a given patient will result in improved outcomes. The dichotomy of PPIs or surgery is being replaced by individualized combinations of interventional and medical therapies. Having an ARP need not mean medical therapy has “failed”, and medication use in conjunction with an ARP may be what is needed for a therapeutic victory. To achieve these goals entails collaboration between surgeons, gastroenterologists, and other specialties.
Figure 1. Depiction of related elements of GERD that result in reduced quality of life. GERD: Gastroesophageal reflux disease.
Clear evidence supports the need for specialization in foregut disease, especially interventional procedures[1]. The American Fellowship Council has an approved foregut surgery fellowship and is developing a similar foregut path for gastroenterologists.
Convergent interventional foregut endoscopy such as per oral endoscopic myotomy, with both surgeons and gastroenterologists performing the procedure, has created a common meeting place for gastroenterologists and surgeons.
STATE OF THE EVIDENCE AND PRECISION MEDICINE
Precision medicine is a medical model that proposes the customization of healthcare, with medical decisions, treatments, practices, or products being tailored to a subgroup of patients, instead of a one-drug-fits-all model[2].
Although randomized controlled trials (RCTs) are considered the “gold standard”, they are increasingly infeasible, and the need for pragmatic trials is advocated by leading gastroenterologists[3]. What constitutes the comparator for new technology is also open to debate: is it PPIs - which are the gold standard medical therapy - or laparoscopic Nissen fundoplication - essentially grandfathered in as no competing technologies existed when introduced?
If GERD is not one disease, there cannot be a “gold standard” treatment. Future research will benefit from this concept. RCT are designed to study equal and therefore homogeneous groups; the endpoints hypothesize superiority of the treatment group. Subset analysis is subsumed in this final endpoint (e.g., one group may have more reflux yet fewer side effects, the conclusion is that both interventions are equal[4,5]). RCTs may be useful in evaluating new therapies. More recent concepts of precision medicine look at defining which therapy is best for a given subgroup. Future research using the precision medicine model is needed to evaluate which ARP is best for a given patient. This will entail changes in research endpoints, methodology, and provider approach to care.
Historical research endpoints and precision medicine
ARP outcomes research has frequently used three measures of outcomes: (1) improvement in GERD-health related quality of life (GERD-HRQL); (2) cessation of daily proton-pump inhibitor (PPI) use; and (3) pH normalization. All three have flaws that should be addressed in future studies to enable individualized therapies.
The symptom which is best relieved by antireflux procedures and least well improved by PPIs, regurgitation, is not assessed by the GERD-HRQL, which has been the most frequently used quality of life assessment in studies of ARPs. Recent studies have measured regurgitation with the Reflux Disease Questionnaire, as well as the Foregut Symptom Questionnaire, the Gastroesophageal Reflux Symptom Scale, and a Regurgitation score adapting the GERD-HRQL grading but substituting “regurgitation” for “heartburn”[6]. Beyond missing the cardinal symptom that best selects patients for ARPs, the GERD-HRQL (and other Quality Of Life surveys) are not designed to evaluate side effects and patient satisfaction carefully, especially in relation to pre-existing patient disease states.
Cessation of PPI use has been an endpoint of almost every study of ARPs. This may seem a reasonable goal for a patient undergoing a more invasive therapy, one relatively easy to assess in study design, and in the current milieu of suspicion of PPI safety is a not infrequent reason for patient consultation. Beyond the flaw that up to 25% of patients resuming PPIs have normal pH tests or may be taking PPIs without clinical benefit (neither of which are routinely assessed in study protocols)[7], it assumes that dual-modality therapy constitutes a failure of an ARP. The majority of patients appropriate for interventional treatment of GERD have an incomplete response to medical therapy (vs. complete response or no response at all). For an intervention to result in a patient who is uncontrolled on medical therapy at baseline to controlled on medical therapy post intervention should be considered a therapeutic victory. Study design going forward should take this into account.
Normalization or improvement of esophageal pH is a valid objective measure that an intervention alters the reflux mechanism and is important in a new technology to validate that symptomatic improvement is not purely a sham effect. However, pH normalization has not been shown to correlate with symptomatic improvement[8]. Improvement in pH as an endpoint also begs the question of whether dual-therapy (intervention + medical therapy) is a reasonable endpoint.
THE DIAPHRAGMATIC SPHINCTER AND TRANSORAL THERAPIES
The ability of the crural muscular sling to create a barrier to reflux was recognized by Allison and Collis; their surgical procedures focused exclusively on restoring the crural sling[9,10]. The importance of restoring the crural sphincter was largely overlooked in the era of fundoplication; repair of the hernia was merely a mechanism to discourage migration of the fundoplication into the chest[11].
To the author’s knowledge, no purely endoscopic therapy has resulted in over 60% long-term normalization of esophageal pH. This may be a limitation of the devices or techniques to enhance the intrinsic lower esophageal sphincter. However, an intriguing and unresolved question regarding purely endoluminal therapies is the degree to which the crural diaphragm must be intact to have a successful result. Traditionally an axial extent of greater than 2 cm has been an exclusion (without any validating studies), although the transverse dimension of the hiatus > 2 cm, and Hill grade 3 or 4 have been proposed as exclusions.
High-resolution manometry has increased our understanding of the crural component of the lower esophageal high-pressure zone. Xiao used 3-D high-resolution impedance manometry (HRIM) to compare 31 pH+ GERD patients without hiatal hernia to 20 controls. Patients with GERD had a significantly lower crural diaphragmatic hiatus apex (DHa) contribution to the high-pressure zone than controls (20.3 vs.
The above studies demonstrating frequent crural deficiencies in patients without a hernia may explain why some patients fail pure endoluminal approaches even when the final result looks satisfactory. A clue may come from a study utilizing high-resolution manometry evaluation of the esophagogastric junction (EGJ) in GERD patients, which found that inspiratory augmentation of the EGJ pressure was the only independent predictive factor associated with GERD, “suggesting that factors independent of lower esophageal sphincter-crural diaphragm (LES-CD) separation are important in maintaining CD function. These factors may be related to the radial dimensions or distensibility of the hiatal canal or the thickness and elasticity of the CD itself[15].”
Crural repair has been demonstrated to restore a significant portion of the reflux barrier. Louie et al. performed intraoperative manometry with separate assessment of pressure and length changes due to crural repair and Nissen fundoplication. Crural repair and fundal wrap contributed equally to increased sphincter length, although crural closure appeared to contribute more to sphincter pressure[16]. Intraoperative functional luminal impedance planimetry (FLIP) evaluation of EGJ distensibility demonstrated that Diaphragmatic re-approximation had a higher percent contribution to distensibility (79% vs. 21%), Cross-Sectional Area (82% vs. 18%), and high pressure zone length (60% vs. 40%) than sphincter augmentation, whether by fundoplication or magnetic sphincter augmentation (MSA)[17].
Clinical confirmation of the importance of restoring the crural sphincter came from studies of MSA. Patients who underwent obligatory dissection and hiatal repair, regardless of the presence of a hiatal hernia, fared better by multiple measures compared to patients without obvious hernia who had MSA placed using minimal dissection without cruroplasty [Table 1][18,19]. These MSA studies and two small studies of transoral incisionless fundoplication (TIF) combined with a laparoscopic hiatal hernia repair[20,21] provide clinical confirmation that failure or inability to restore the crural sphincter may be an inherent limitation of endoscopic therapies, regardless of the presence or absence of a hiatal hernia.
Patients who underwent obligatory dissection with hiatal repair, regardless of absence or presence of a hiatal hernia, fared better by multiple measures compared to patients without obvious hernia who had MSA placed using minimal dissection without cruroplasty[16,17]
| Minimal dissection | Obligatory repair | |
| Recurrent GERD | 17.1% | 2.3% |
| New-onset dysphagia | 7.1% | 0% |
| EGD device herniation | 9.6% | 0.0% |
| EGD recurrent/persistent hiatal hernia | 8.3% | 0.0% |
| EGD recurrent/persistent hiatal hernia > 2 cm | 8.3% | 3.7% |
| Device removed | 8.3% | 3.7% |
| Repeat hiatal hernia repair +/- LINX removal | 6.6% | 0.0% |
C-TIF (combined TIF)
The intriguing concept of combining a laparoscopic hiatal dissection and repair with a transoral fundoplication (C-TIF) has opened avenues for discussion and collaboration between gastroenterologists and surgeons. Whether the results will surpass a laparoscopic partial fundoplication in terms of success, durability, and side effects remains to be seen. Endoscopic TIF has a minimal side effect profile regarding dysphagia and gas-bloat similar to that seen with a 90-to-120-degree fundoplication[22]. An ongoing study comparing C-TIF to laparoscopic Nissen fundoplication (ClinicalTrials.gov NCT04795934) will help answer these questions, though some would argue the better comparator would be to a partial 90-to-120-degree laparoscopic fundoplication.
CALIBRATION OF THE HIATAL REPAIR
Recognizing the importance of restoring the crural sphincter brings about new questions regarding calibration of the hiatal repair during laparoscopic surgery. Historically laparoscopic techniques relied on a bougie or visual inspection of the hiatus with an undistended esophagus to size the hiatal repair. Given the supra-physiologic efficacy of a Nissen or partial fundoplication, the goal was to minimize the potential for recurrence without risking dysphagia[23]. The robustness and laxity of the crura vary greatly between patients, consistent with the recognition of a connective tissue defect in GERD patients[24]. Methods to assess the distensibility utilizing impedance planimetry (EndoFLIP) may have a role in appropriate calibration of the repair[25].
FUTURE TECHNOLOGIES
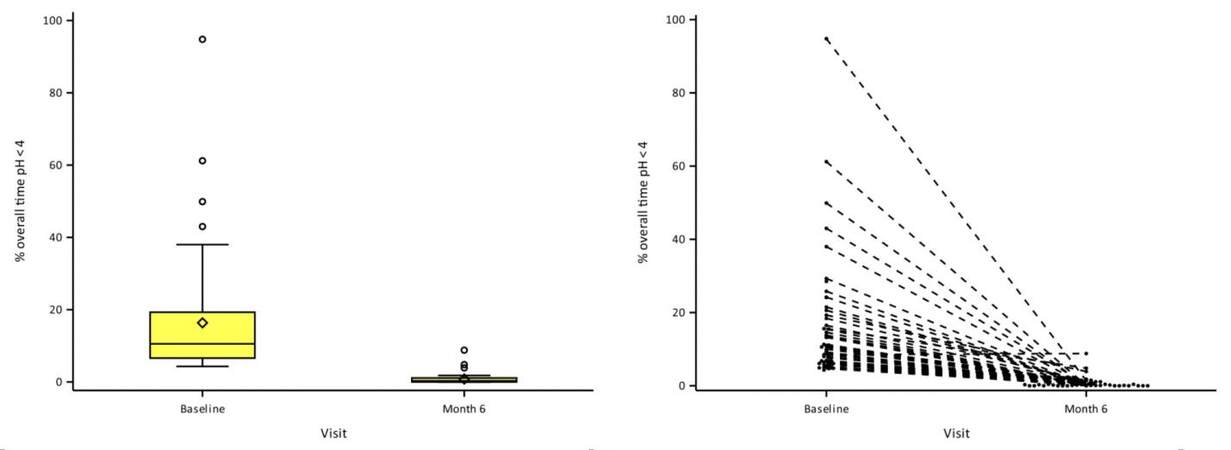
A novel implant [RefluxStopTM (Implantica, Zug, Switzerland)] has undergone clinical trials in Europe with promising early results [Figure 2].
Figure 2. RefluxStop 24-h pH monitoring at baseline and 6 months post-opera = on. 24-h pH monitoring mean reduc = on from baseline of 16.35% to 0.80% at 6-month visit. Normal 24-h pH results in 98% of subjects. From Bjelovic et al. permission obtained for publication[26].
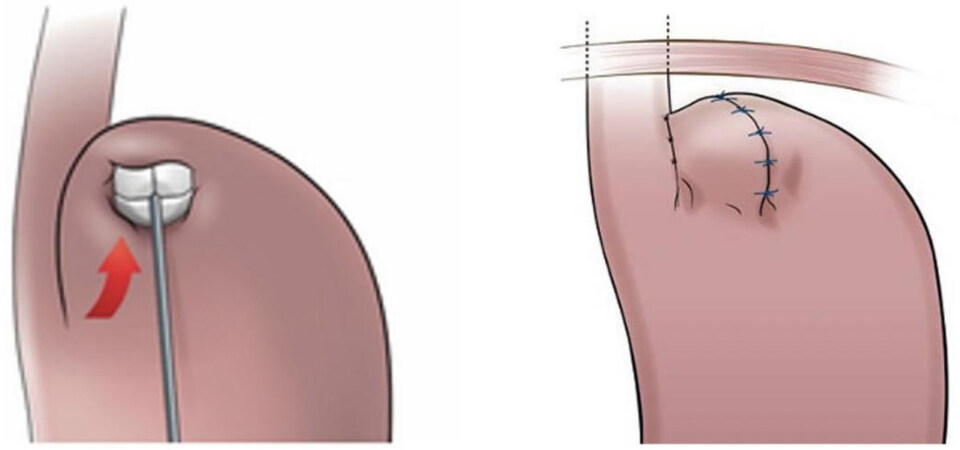
RefluxStopTM aims to block the movement of the lower esophageal sphincter (LES) up into the thorax and keep the angle of His in its original, anatomically correct position [Figure 3][26].
Figure 3. the RefluxStop device is positioned at the fundus and enclosed by sutures. From Bjelovic et al..permission obtained for publication[26].
Devices placed with laparoscopic surgery around the lower esophageal sphincter designed to have a similar physiologic function as the magnetic sphincter augmentation device (LINX®) have been considered; to the author’s knowledge, none are under human investigation at this time.
Robotic surgery using platforms such as the DaVinci have the potential to improve high mediastinal dissection. Robotic simulators can build skills outside the operating room, and ergonomics can lengthen a surgeon’s career. Computer-assisted analysis may enable better reproducibility of procedures.
New robotic endoscopic devices may provide the technical prowess to perform endoscopic hiatal hernia repair. If they do, it will be a game-changer in the potential for purely endoscopic ARPs.
DISCUSSION
With the premise that a given ARP provides reasonable control of reflux, then personalized selection of the appropriate ARP will involve understanding patient symptoms and expectations, potential side effects, invasiveness, durability, disease seriousness, response to medical therapy, and severity of injury among other factors.
Study endpoints must be reevaluated. Resumption or continuation of medical therapy post an antireflux procedure is not a failure if the combination therapy results in a better outcome than either alone. Quality of life surveys designed to precisely evaluate the side effects of therapy are needed. Subset analysis is key to precision medicine and requires pragmatic trials, not RCTs.
Foregut medicine is a specialty that requires the multidisciplinary approach of societies such as the American Foregut Society and European Foregut Society. Specialization will provide new insights into best practices for personalized care and foster the expertise needed for optimal care of GERD patients.
DECLARATIONS
Authors’ contributionsThe author contributed solely to the article.
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestThe author declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Khoshhal Z, Canner J, Schneider E, et al. Impact of surgeon specialty on perioperative outcomes of surgery for benign esophageal diseases: a NSQIP analysis. J Laparoendosc Adv Surg Tech A 2017;27:924-30.
2. . Toward precision medicine: building a knowledge network for biomedical research and a new taxonomy of disease. Washington (DC): National Academies Press (US); 2011.
3. Yadlapati R, Pandolfino JE. Medical versus surgical treatment for refractory heartburn. N Engl J Med 2020;382:296-7.
4. Lundell L, Attwood S, Ell C, et al. Comparing laparoscopic antireflux surgery with esomeprazole in the management of patients with chronic gastro-oesophageal reflux disease: a 3-year interim analysis of the LOTUS trial. Gut 2008;57:1207-13.
5. Rudolph-Stringer V, Bright T, Irvine T, et al. Randomized trial of laparoscopic nissen versus anterior 180 degree partial fundoplication - late clinical outcomes at 15 to 20 years. Ann Surg 2022;275:39-44.
6. Bell R, Lipham J, Louie BE, et al. Magnetic sphincter augmentation superior to proton pump inhibitors for regurgitation in a 1-year randomized trial. Clin Gastroenterol Hepatol 2020;18:1736-43.e2.
7. Lord RV, Kaminski A, Oberg S, et al. Absence of gastroesophageal reflux disease in a majority of patients taking acid suppression medications after Nissen fundoplication. J Gastrointest Surg 2002;6:3-9; discussion 10.
8. Bell RC, Fox MA, Barnes WE, et al. Univariate and multivariate analyses of preoperative factors influencing symptomatic outcomes of transoral fundoplication. Surg Endosc 2014;28:2949-58.
9. Allison PR. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg Gynecol Obstet 1951;92:419-31.
11. Nissen R, Rossetti M. Surgery of hiatal and other diaphragmatic hernias. J Int Coll Surg 1965;43:663-74.
12. Xiao Y, Lin Z, Li Y, Pandolfino JE, Chen M, Kahrilas PJ. Correlation between novel 3D high-resolution manometry esophagogastric junction metrics and pH-metry in reflux disease patients. Neurogastroenterol Moti 2018;30:e13344.
13. MA ES, Nobre RA, Bezerra PC, Dos Santos AA, Sifrim D. Anatomical and functional deficiencies of the crural diaphragm in patients with esophagitis. Neurogastroenterol Motil 2017:29.
14. Masuda T, Singhal S, Akimoto S, Bremner RM, Mittal SK. Swallow-induced esophageal shortening in patients without hiatal hernia is associated with gastroesophageal reflux. Dis Esophagus 2018:31.
15. Pandolfino JE, Kim H, Ghosh SK, Clarke JO, Zhang Q, Kahrilas PJ. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol 2007;102:1056-63.
16. Louie BE, Kapur S, Blitz M, Farivar AS, Vallieres E, Aye RW. Length and pressure of the reconstructed lower esophageal sphincter is determined by both crural closure and Nissen fundoplication. J Gastrointest Surg 2013;17:236-43.
17. Stefanova DI, Limberg JN, Ullmann TM, et al. Quantifying factors essential to the integrity of the esophagogastric junction during antireflux procedures. Ann Surg 2020;272:488-94.
18. Tatum JM, Alicuben E, Bildzukewicz N, Samakar K, Houghton CC, Lipham JC. Minimal versus obligatory dissection of the diaphragmatic hiatus during magnetic sphincter augmentation surgery. Surg Endosc 2019;33:782-8.
19. Schwameis K, Nikolic M, Castellano DGM, et al. Crural closure improves outcomes of magnetic sphincter augmentation in GERD patients with hiatal hernia. Sci Rep 2018;8:7319.
20. Ihde GM, 2nd, Pena C, Scitern C, Brewer S. pH scores in hiatal repair with transoral incisionless fundoplication. JSLS 2019;23:e2018.00087.
21. Choi AY, Roccato MK, Samarasena JB, et al. Novel interdisciplinary approach to GERD: concomitant laparoscopic hiatal hernia repair with transoral incisionless fundoplication. J Am Coll Surg 2021;232:309-18.
22. Shukri MJ, Watson DI, Lally CJ, Devitt PG, Jamieson GG. Laparoscopic anterior 90 degree fundoplication for reflux or large hiatus hernia. ANZ J Surg 2008;78:123-7.
24. Fei L, del Genio G, Brusciano L, et al. Crura ultrastructural alterations in patients with hiatal hernia: a pilot study. Surg Endosc 2007;21:907-11.
25. Su B, Novak S, Callahan ZM, Kuchta K, Carbray J, Ujiki MB. Using impedance planimetry (EndoFLIP) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg Endosc 2020;34:1761-8.
26. Bjelovic M, Harsanyi L, Altorjay A, Kincses Z, Forsell P. Investigators of the RefluxStop Clinical Investigation Study G. Non-active implantable device treating acid reflux with a new dynamic treatment approach: 1-year results : RefluxStopTM device; a new method in acid reflux surgery obtaining CE mark. BMC Surg 2020;20:159.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Bell R. State of evidence and future perspectives in minimally invasive management of gastroesophageal reflux disease (GERD). Mini-invasive Surg 2022;6:42. http://dx.doi.org/10.20517/2574-1225.2022.20
AMA Style
Bell R. State of evidence and future perspectives in minimally invasive management of gastroesophageal reflux disease (GERD). Mini-invasive Surgery. 2022; 6: 42. http://dx.doi.org/10.20517/2574-1225.2022.20
Chicago/Turabian Style
Bell, Reginald. 2022. "State of evidence and future perspectives in minimally invasive management of gastroesophageal reflux disease (GERD)" Mini-invasive Surgery. 6: 42. http://dx.doi.org/10.20517/2574-1225.2022.20
ACS Style
Bell, R. State of evidence and future perspectives in minimally invasive management of gastroesophageal reflux disease (GERD). Mini-invasive. Surg. 2022, 6, 42. http://dx.doi.org/10.20517/2574-1225.2022.20
About This Article
Copyright
Data & Comments
Data
 Cite This Article 12 clicks
Cite This Article 12 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.